In this post, JBJS Editor-in-Chief Dr. Marc Swiontkowski discusses a new study on time to debridement of open femoral and tibial fractures and infection risk. The retrospective analysis drew from the SIGN (Surgical Implant Generation Network) Surgical Database, a large prospective registry of fracture cases in predominantly low-resource settings.
The Surgical Implant Generation Network (SIGN) was founded by Dr. Lewis Zirkle in Richland, Washington in the late 1990s. Based on his experiences serving in the Vietnam War and subsequent visits to Vietnam and other countries, he desired to develop a relatively low-cost intramedullary implant that could be inserted without fluoroscopy, which is often not available in low-resource settings. The SIGN nail is offered free of charge to surgeons in these settings. The “deal” that is agreed to is that the surgeon will provide pre- and postoperative radiographs and clinical follow-up data to the SIGN database. Last week, OrthoBuzz published a post on one study that used the SIGN Fracture Care International database: IMN Fixation for Femoral Nonunion in Pediatric Patients in Lower Resource Countries.
In a separate study in the October 18, 2023 issue of JBJS, Cortez et al. report on the database outcomes of >10,000 open fractures of the tibia and femur in patients ≥16 years of age who were treated with a SIGN intramedullary nail:
Delays in Debridement of Open Femoral and Tibial Fractures Increase Risk of Infection
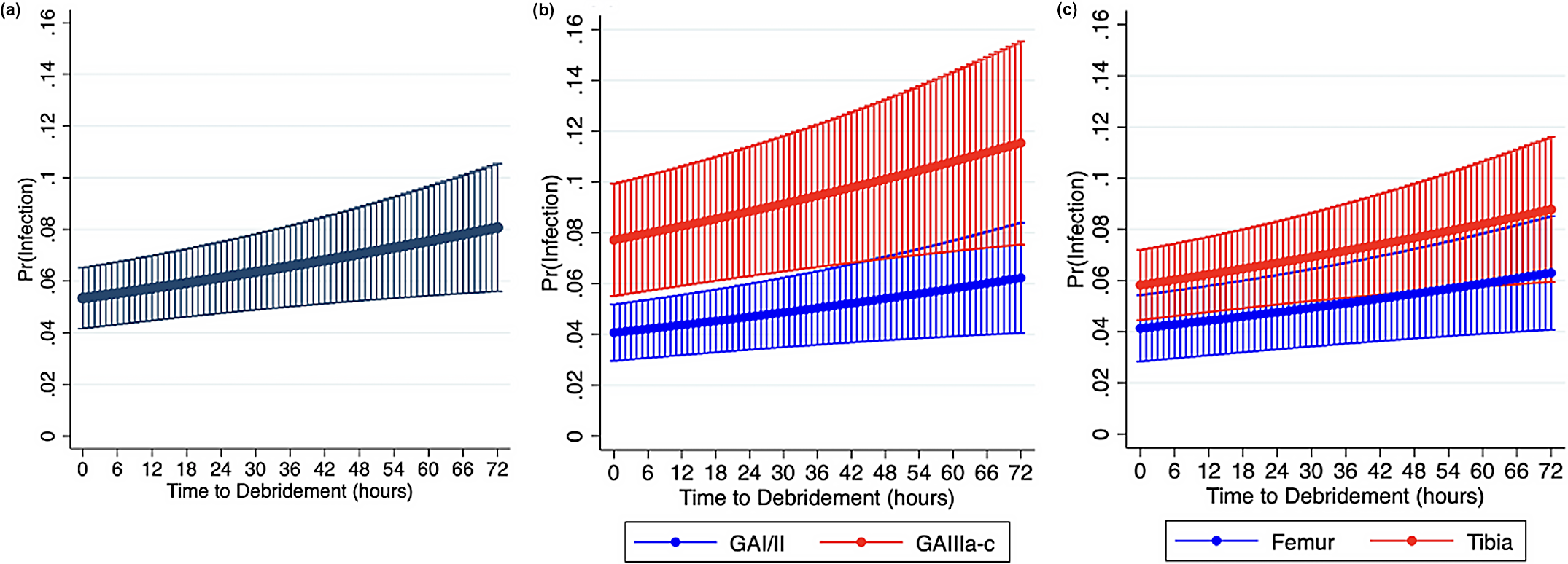
The authors sought to evaluate the probability of infection with increasing time to debridement (in 6-hour increments). They report that follow-up-related criteria were met for 27% of the 39,075 fractures initially identified. The included patients were from 61 countries.
One limitation related to the methodology is that the time from injury to initial debridement was an estimated value based on patient recall at presentation. Additionally, the reporting of the administration of perioperative antibiotics was inconsistent in the database, and thus these data were not included in the analysis. Patients not treated with debridement within 7 days were excluded.
The findings confirm what is known in the management of these long-bone fractures in more resource-rich environments. These findings include fractures involving the tibia being at greater risk of infection than those in the femur, and higher grade injuries (Gustilo-Anderson type III vs. type I or II) being at greater risk of infection. Moreover, the investigators found that for every 6-hour delay to debridement, the risk of infection increased by 0.17%.
Despite the methodologic limitations, this research informs the call to action by many in the worldwide community to address issues regarding transportation to treatment centers as a top priority. Such issues may best be addressed locally with input from treating centers to governmental decision-makers. Nonetheless, these data on lower-extremity fractures, and the mechanism to record and report them, can be revisited every 2 to 3 years to evaluate progress in treating these common injuries. As the authors note, the large size and international nature of the cohort in this study make the findings “uniquely generalizable” across environments.
Read the full study at JBJS.org: Delays in Debridement of Open Femoral and Tibial Fractures Increase Risk of Infection
Additional perspective on this study is provided in a commentary article by Patrick C. Schottel, MD: Is Time Really of the Essence for Open Fracture Debridement?
JBJS Editor-in-Chief