In November 2023, leaders of the editorial boards of 6 orthopaedic journals, leaders of funding agencies, and officials from the National Institutes of Health met

In this post, Deputy Editor for Social Media Matt Schmitz discusses a study by Sato et al. now available in JBJS. Developmental dysplasia of the

JBJS is pleased to welcome Dr. Mohit (Mo) Bhandari as our new Editor-in-Chief. Dr. Bhandari succeeds Dr. Marc Swiontkowski, who has served as Editor-in-Chief since
A video abstract is available with the new report in JBJS by the Major Extremity Trauma Research Consortium (METRC): The Bioburden Associated with Severe Open
Severe hip OA linked to worse functional impairment even after spinal surgery, reports Journal of Bone & Joint Surgery Newswise — Waltham — April 30, 2024 — One-third of
The JBJS Clinical Summaries collection continues to expand. The summaries are a useful tool for musculoskeletal clinicians, offering synopses of recent findings and current treatment

This Resident Roundup post comes from Mike Kim, MD, an incoming intern in the Department of Orthopaedic Surgery at the University of California, Irvine School

Topics of interest in foot and ankle surgery, including hallux valgus recurrence, simultaneous vs. sequential total ankle arthroplasty (TAA), and more, are featured in the

The JBJS community extends its sincere thanks to Dr. Marc Swiontkowski for his steadfast and dedicated leadership as Editor-in-Chief over the past decade. As announced
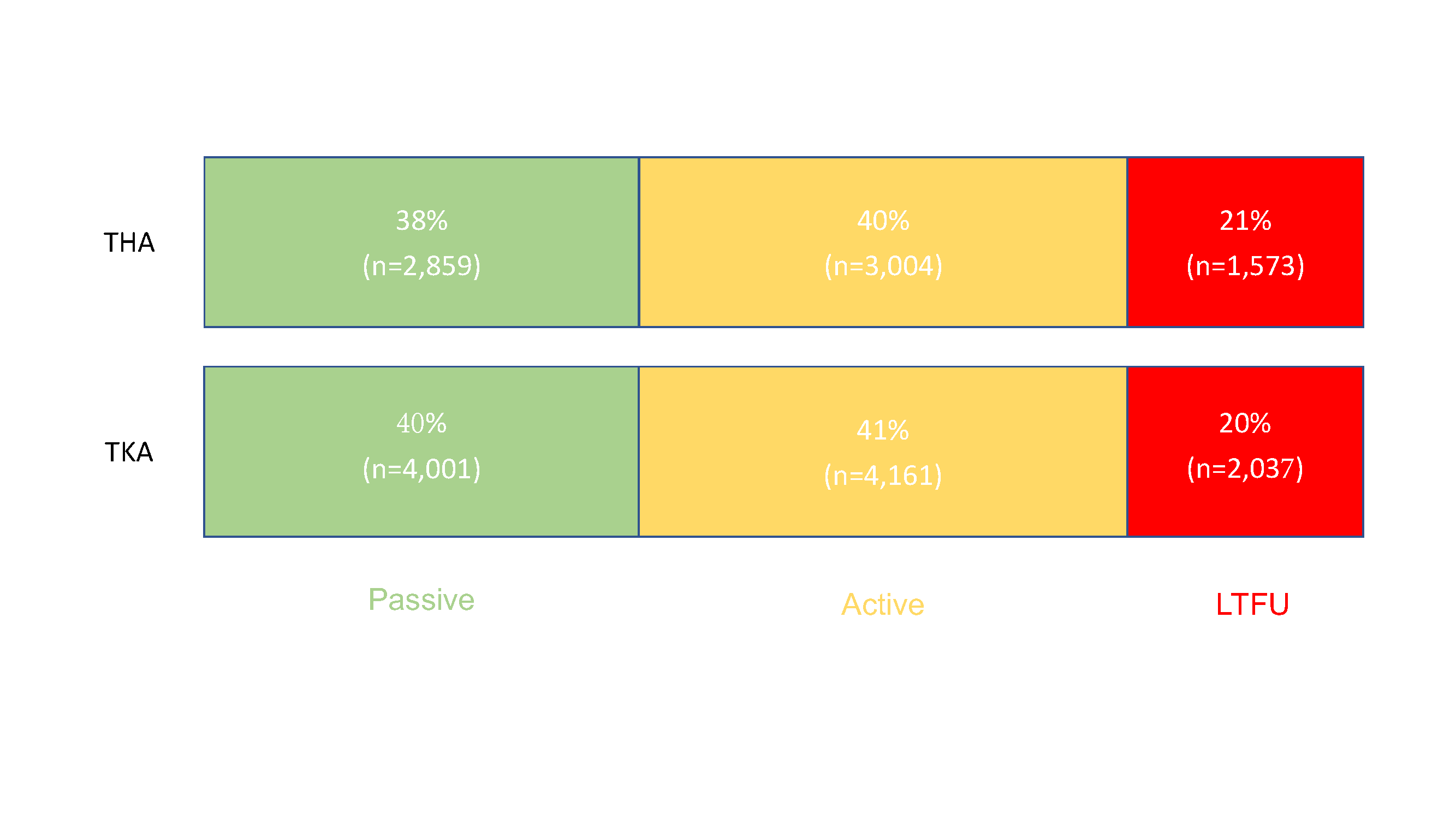
Editor-in-Chief Dr. Marc Swiontkowski reflects on a new study that examines the capture of patient-reported outcome measures (PROMs) after total joint arthroplasty. He offers a