JBJS Clinical Classroom continues to grow as a learning hub. Clinical Classroom subscribers now have access to JBJS Chapman’s Comprehensive Orthopaedic Surgery, an indispensable resource

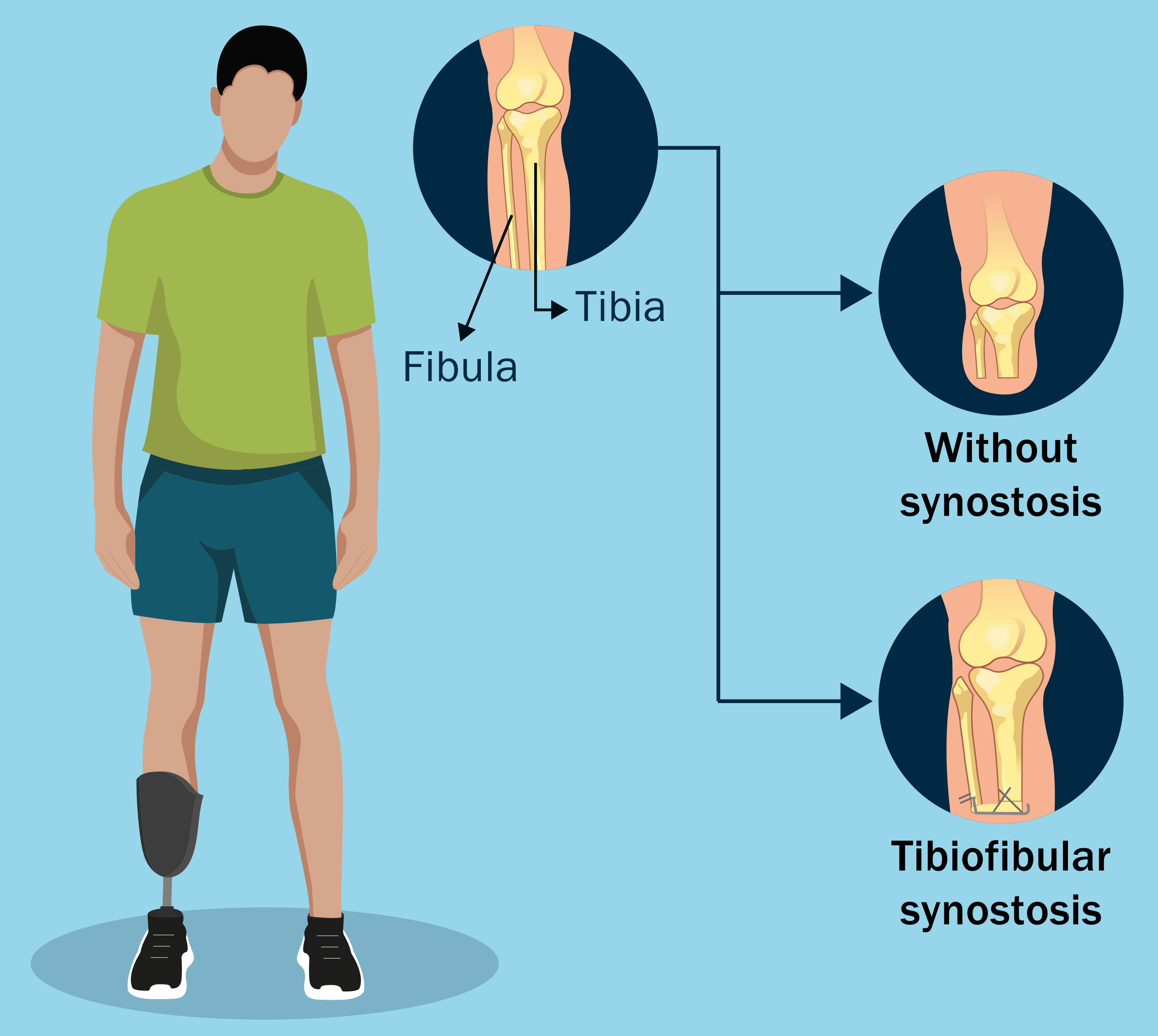
Topics of interest in adult reconstructive knee surgery are presented in the new JBJS Guest Editorial What’s New in Adult Reconstructive Knee Surgery. Here, we
Dr. Matt Schmitz, JBJS Deputy Editor for Social Media, discusses 3 recent studies that reflect the rigorous standards, and challenges, of randomized clinical trials (RCTs).
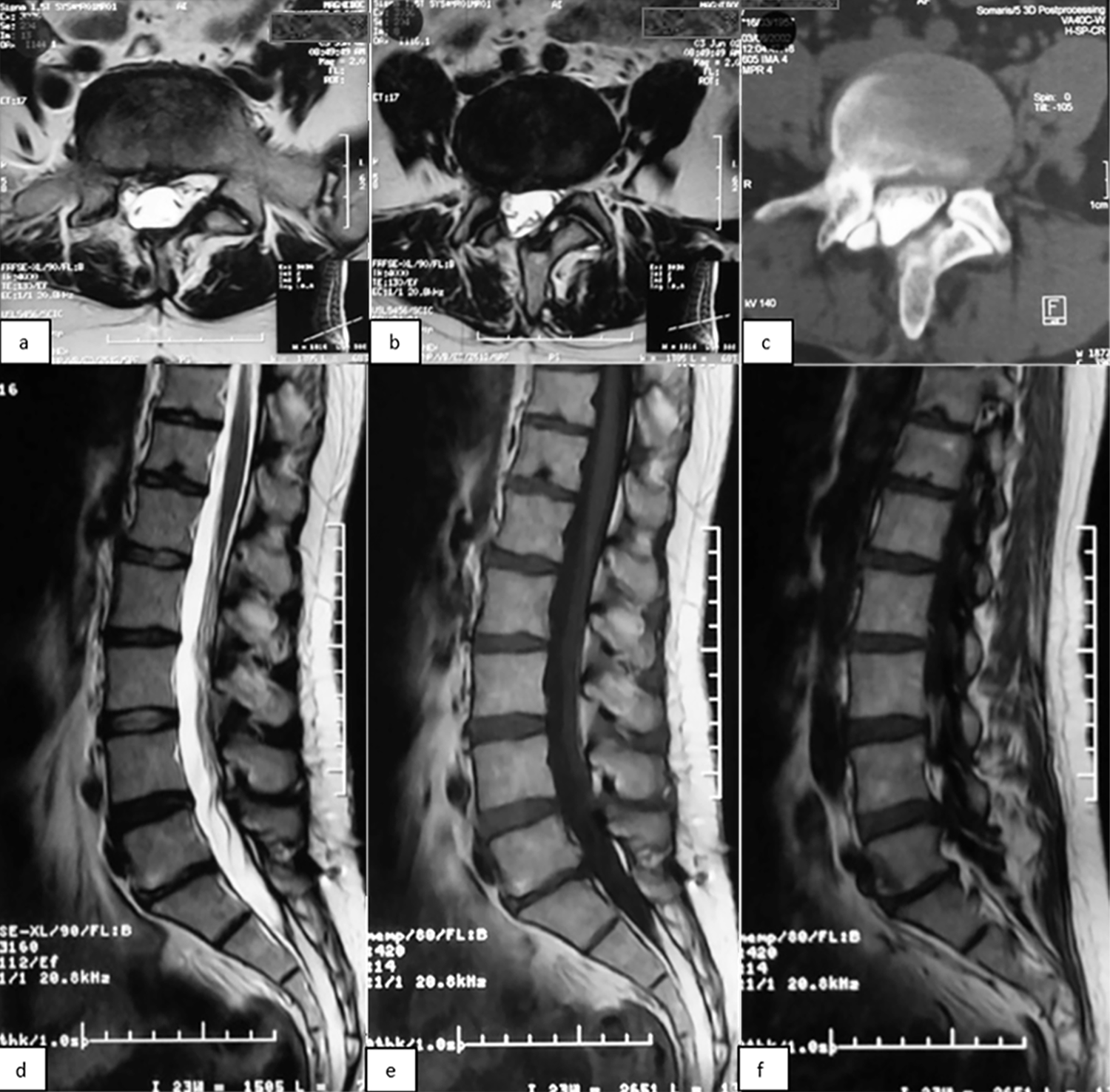
Investigators in France evaluated the long-term outcomes of 1- and 2-level total disc arthroplasty (TDA) in patients with chronic lumbar degenerative disc disease. A total
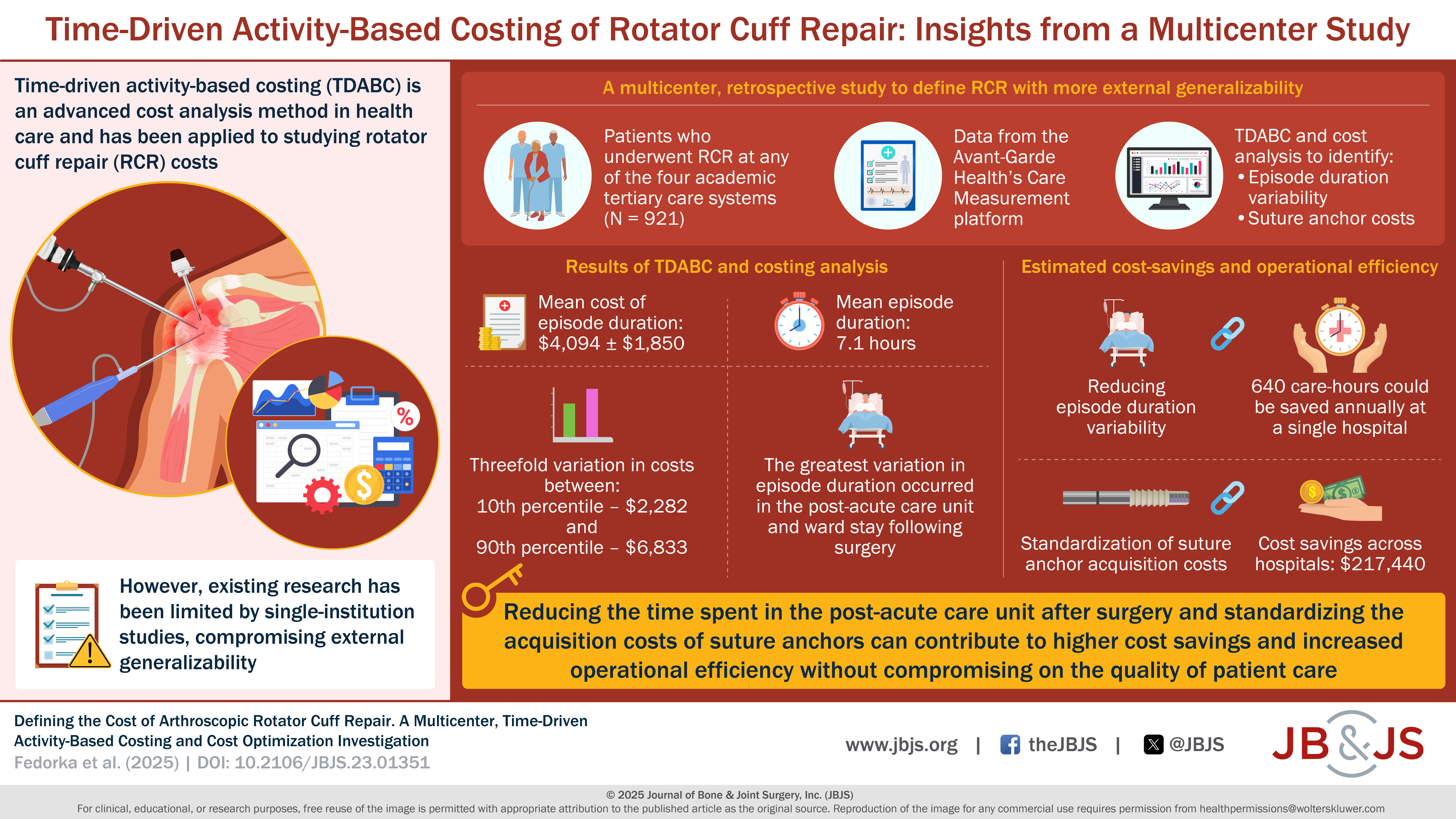
In a study now published in JBJS, Fedorka et al. evaluate the cost of rotator cuff repair (RCR) using time-driven activity-based costing (TDABC). This methodology,

In this post, OrthoBuzz spotlights JBJS video and audio content connecting members of the orthopaedic community around the globe. Video JBJS Essential Surgical Techniques (EST)
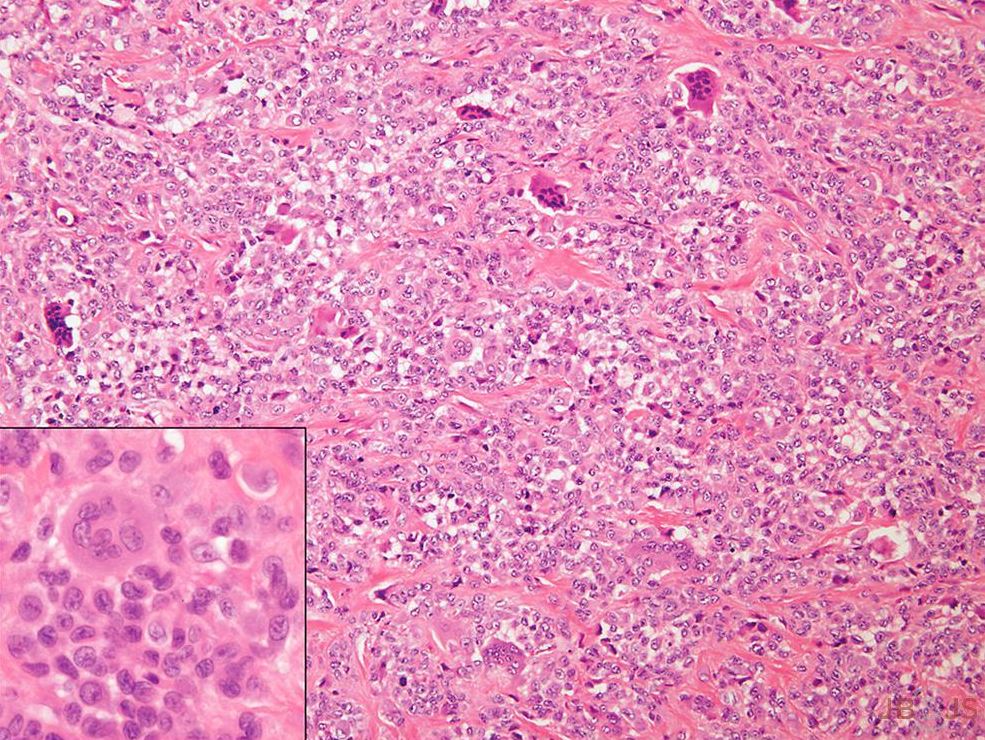
Key topics in orthopaedic oncology are discussed in the new JBJS Guest Editorial What’s New in Musculoskeletal Tumor Surgery. Here, we highlight studies of high

The rigorous evaluation of manuscripts submitted to JBJS would not be possible without the many Consultant Reviewers from around the world who contribute their knowledge

HIP ATTACK data show elevated troponin in 1 in 5 hip fracture patients, reports a new study in JBJS. For hip fracture patients with

The OrthoJOE podcast is celebrating its 100th episode. You can access the milestone episode and the full OrthoJOE archive here. Launched in 2021 as a