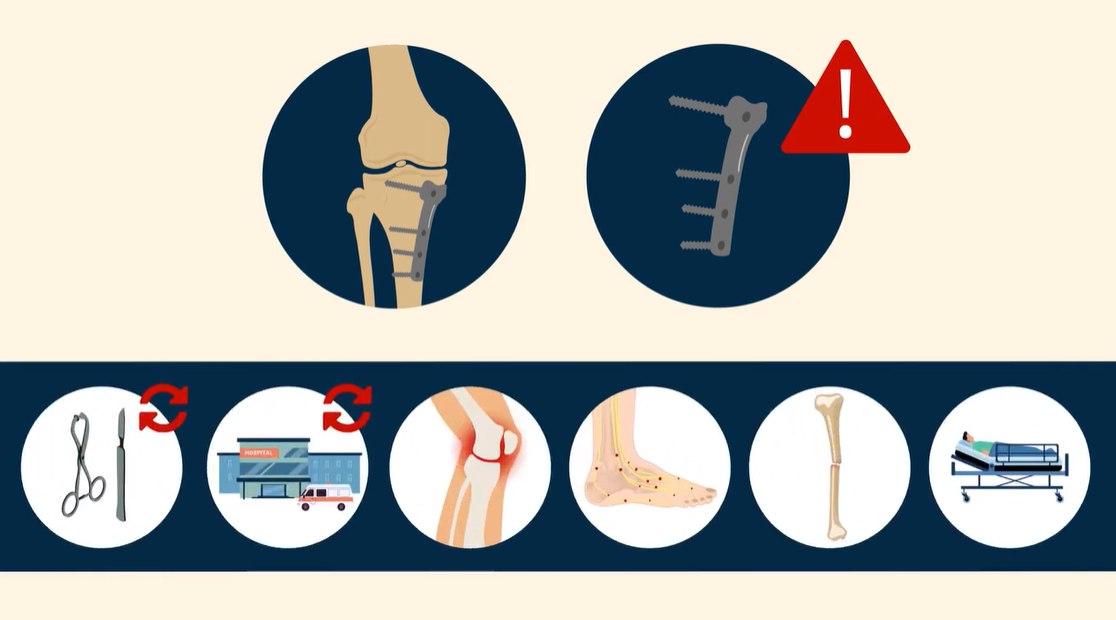
The removal of metal fixation devices (hardware removal) is one of the 10 most frequently performed surgical procedures in orthopaedics. To the surgeon with limited experience, these procedures can appear to be straightforward and
Tag: ABOS
This guest post comes from David Vizurraga, MD in response to a recent JBJS Orthopaedic Forum article. Additional perspective on this topic is provided by JBJS Editor-in-Chief Dr.
One goal of an orthopaedic surgery residency is to prepare residents for the procedures they will perform when they are attendings. Yet, until the retrospective
Hip arthroscopy for labral pathology and cam and pincer impingement has become increasingly established as an effective procedure in the hands of experienced surgeons. However,
The new second-quarter 2017 JBJS Quarterly CME Exam—based on articles published in April, May, and June 2017—is now available. This course contains 100 assessment questions on
The first 2016 JBJS Quarterly CME Exam—based on articles published in January, February, and March—is now available. Starting now and going forward, each interactive quarterly