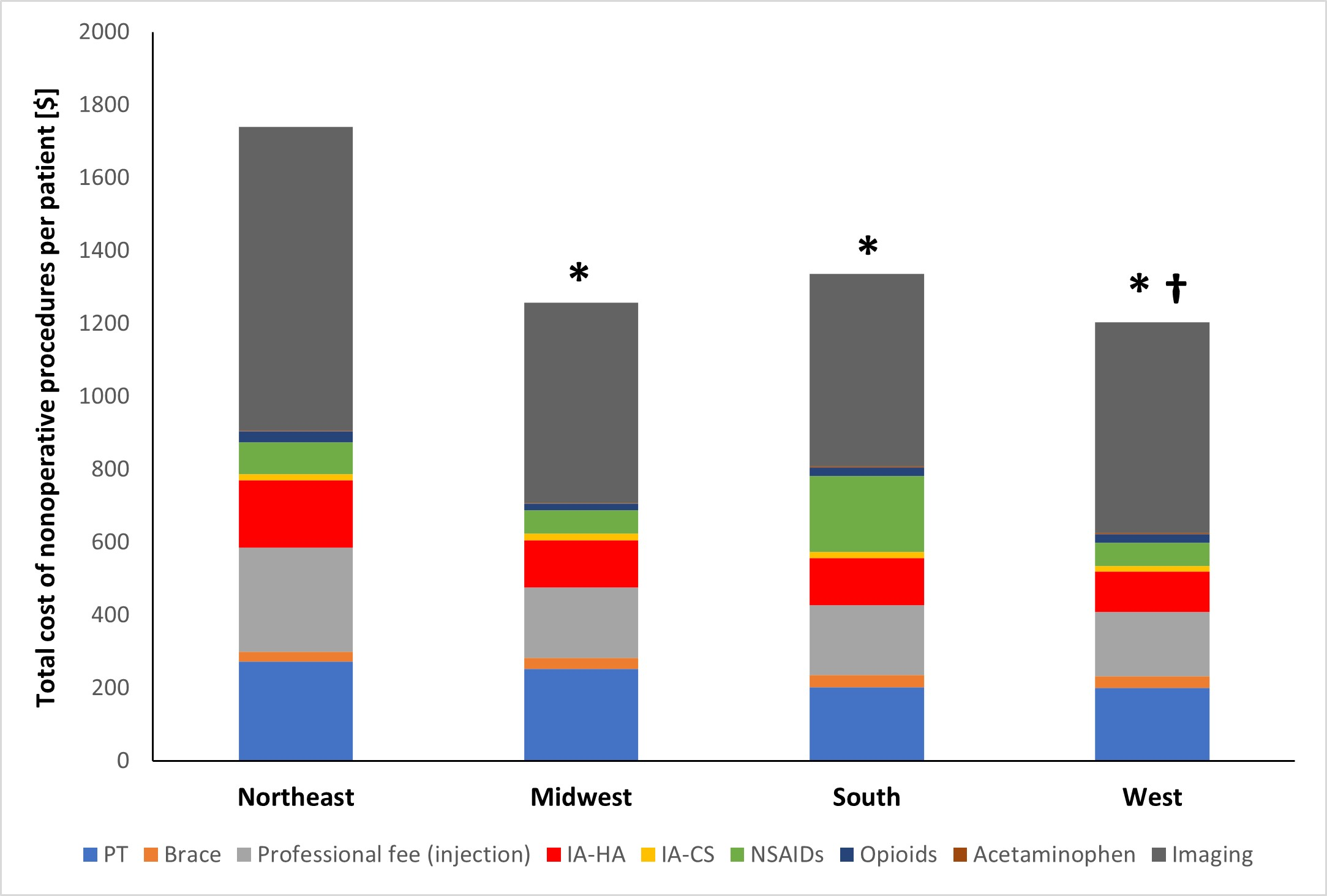
A new JBJS study reviews costs associated with nonoperative management of osteoarthritis in the 1-year period leading up to total knee arthroplasty (TKA). JBJS Deputy
Tag: Acetaminophen
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Eric Secrist, MD in response to a recent study in Arthritis Research & Therapy.
As if on cue, a just-published study in JAMA backed up the recent AAOS statement on opioids by finding that neither the opiate oxycodone nor
Many orthopaedists and primary care clinicians recommend acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) as a first-line approach for patients with osteoarthritis (OA) or back pain.