In this OrthoBuzz post, Editor-in-Chief Dr. Marc Swiontkowski reflects on a new JBJS study that examines pain catastrophizing among patients with adolescent idiopathic scoliosis (AIS).
Tag: adolescent idiopathic scoliosis
As we continue to evaluate methods of treating adolescent idiopathic scoliosis (AIS), growth modulation has become a hot topic. Such techniques aim at curve correction without the need for fusion, and can involve either tethering on the convex side of the curve or distraction on the concave
JBJS is pleased to highlight the orthopaedic residents who help implement the Robert Bucholz Resident Journal Club Grants at their institutions. The grant program promotes career-long

Every month, JBJS publishes a review of the most pertinent and impactful studies reported in the orthopaedic literature during the previous year in 14 subspecialties. Click here for a collection of
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 14 specialty areas. Click here for
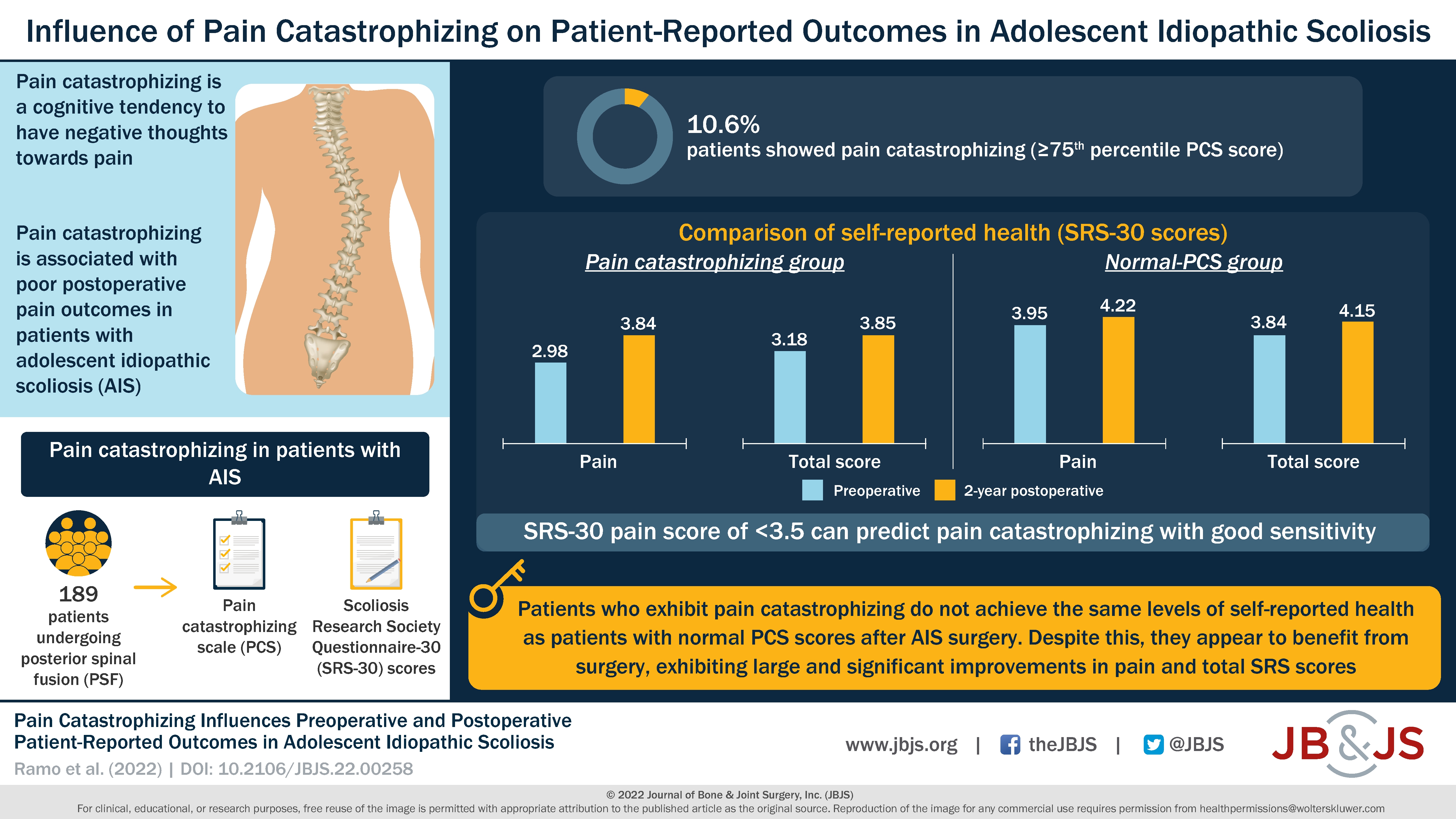
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Impact Science, in response to a recent article in JBJS. Pain management is an important
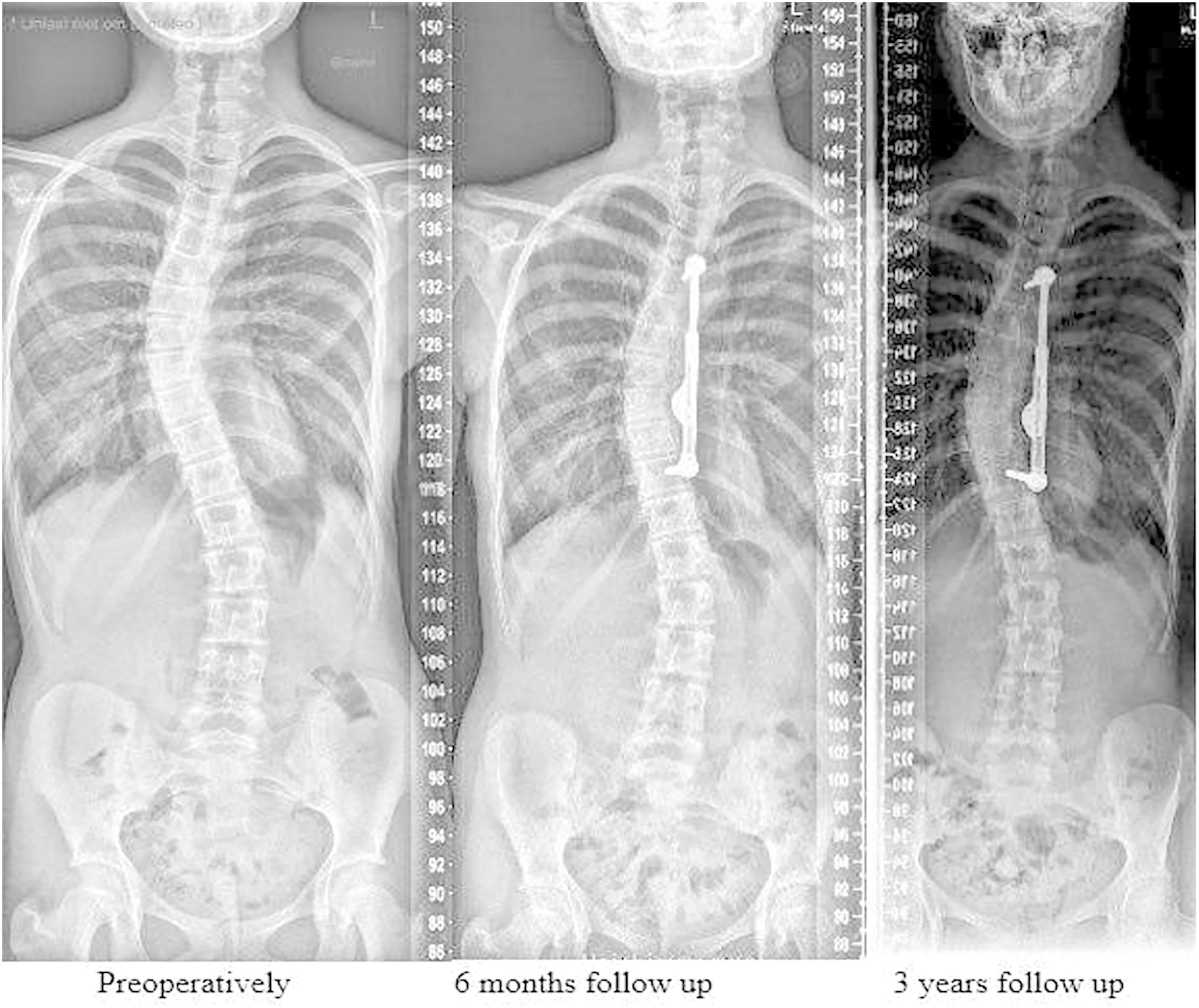
The tried-and-true treatment for progressive adolescent idiopathic scoliosis (AIS) is a posterior spinal fusion (PSF). However, for skeletally immature patients, there is increasing interest in
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for
The evidence favoring tranexamic acid (TXA) for reducing surgical blood loss is ample and growing, but until now robust data were sparse regarding its efficacy
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click