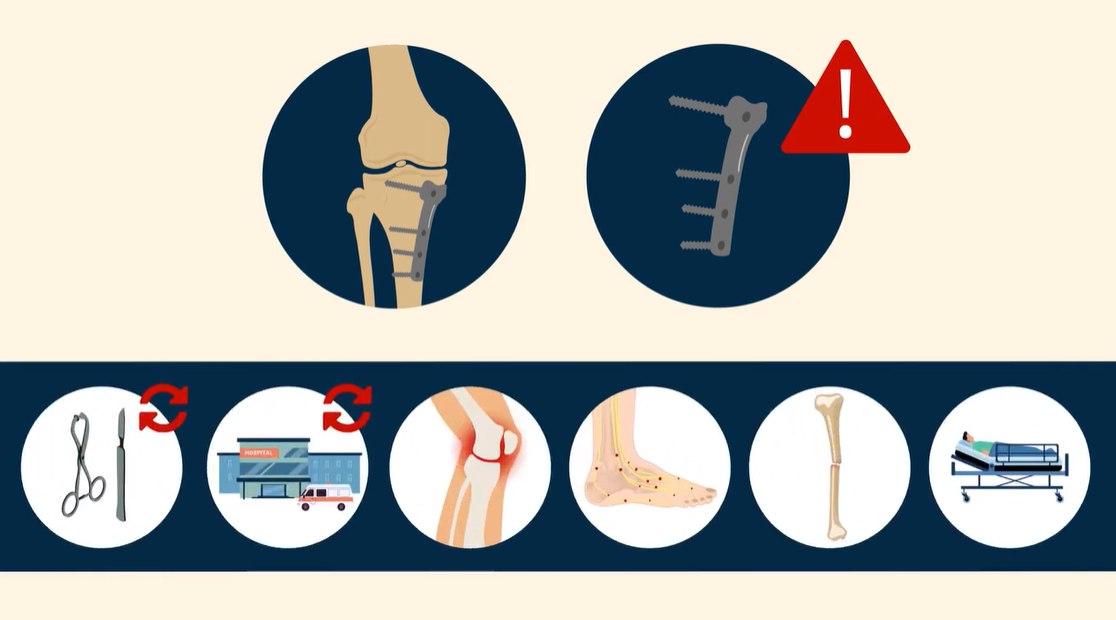
The removal of metal fixation devices (hardware removal) is one of the 10 most frequently performed surgical procedures in orthopaedics. To the surgeon with limited experience, these procedures can appear to be straightforward and
Tag: American Board of Orthopaedic Surgery
This guest post comes from David Vizurraga, MD in response to a recent JBJS Orthopaedic Forum article. Additional perspective on this topic is provided by JBJS Editor-in-Chief Dr.
Increasingly, the care of patients with musculoskeletal problems is being provided by teams of providers with varied professional backgrounds and diverse types of experience. On
In the May 20, 2015 edition of The Journal of Bone & Joint Surgery, Horst et al. document the increasing subspecialization of orthopaedic residency graduates