Orthopaedic colleagues who live and practice in low-resource areas around the world have clearly voiced that they want support from better-resourced partners. But such efforts
Tag: ankle
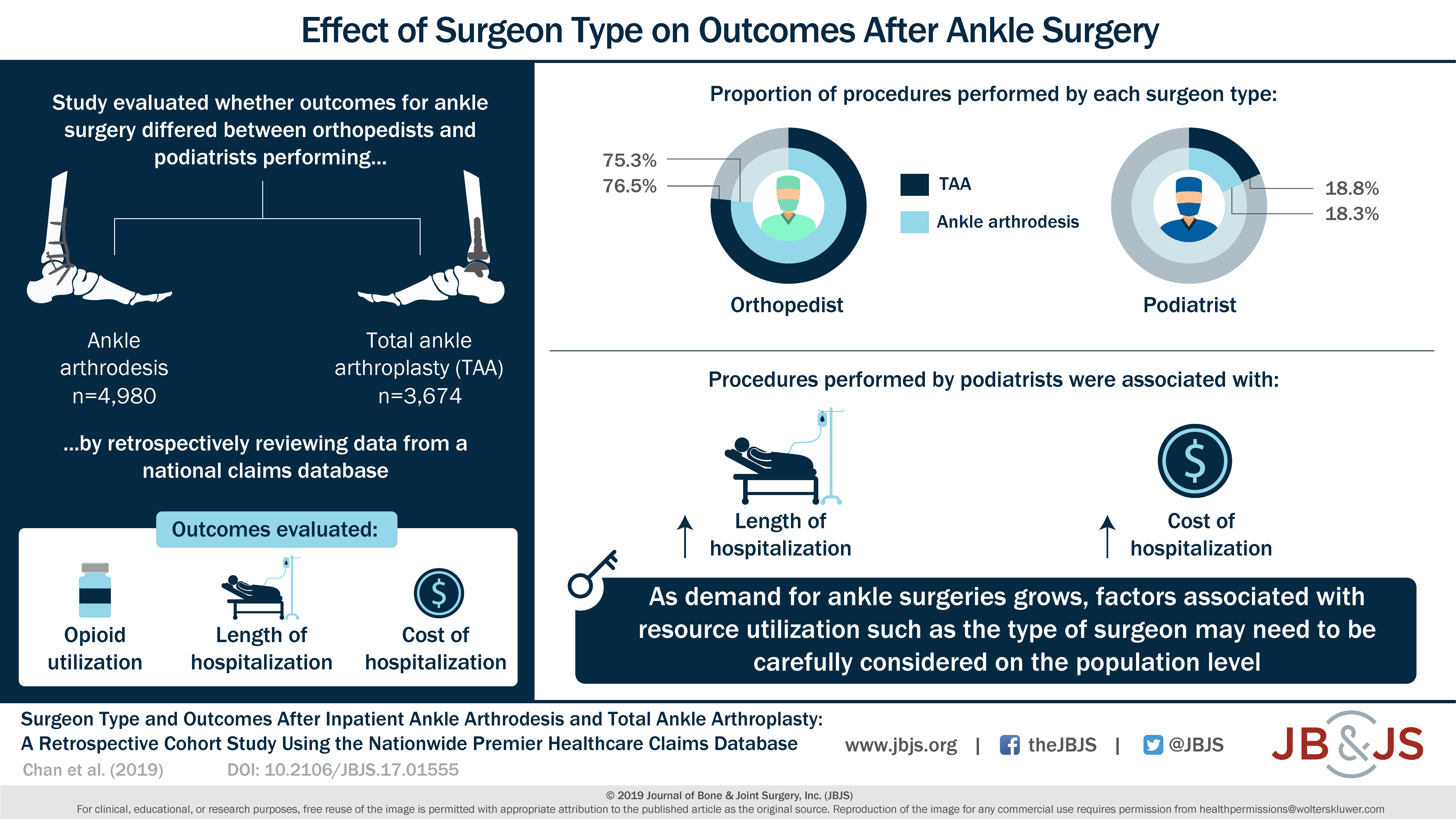
Full Article Background: Two main treatments for end-stage ankle arthritis are ankle arthrodesis and total ankle arthroplasty (TAA). While both procedures can be performed either
Full Article Background:To our knowledge, there are no reports of the Ponseti method initiated after walking age and with >10 years of follow-up. Our goal
The Intrepid Dynamic Exoskeletal Orthosis (IDEO) is a custom energy-storing carbon fiber ankle-foot orthosis developed for lower-extremity trauma patients. Studies conducted at the military treatment
Up to 40% of patients with idiopathic clubfoot who are treated with the Ponseti method experience recurrence of deformity. https://bit.ly/2IuVOm1 Related video from JBJS Essential Surgical
Occasionally, patients experience new or increased ankle pain following total knee arthroplasty (TKA). https://bit.ly/2IkLoGD #JBJS #JBJSVideoSummaries
Childhood toe-walking is usually a transient condition. https://bit.ly/2Fegj4Z #JBJS
Ankle sprain is a common musculoskeletal injury throughout the world, affecting tens of thousands of patients daily. What treatments for lateral inversion ankle injury are
OrthoBuzz regularly brings you a current commentary on a “classic” article from The Journal of Bone & Joint Surgery. These articles have been selected by the
We have entered an era where total ankle arthroplasty (TAA) is accepted as a rational approach for patients with degenerative arthritis of the ankle. TAA
