Co-author Rachel M. Frank, MD summarizes the 5 most compelling findings from among the studies highlighted in the new “What’s New in Sports Medicine” in JBJS.
Tag: Anterior cruciate ligament

A randomized clinical trial remains at the top of the Level of Evidence pyramid precisely because this experimental design is the optimum way to limit
Anterior cruciate ligament (ACL) injuries once were career-ending for athletes. With the advent of ACL reconstruction, elite athletes have been able to continue to compete at the
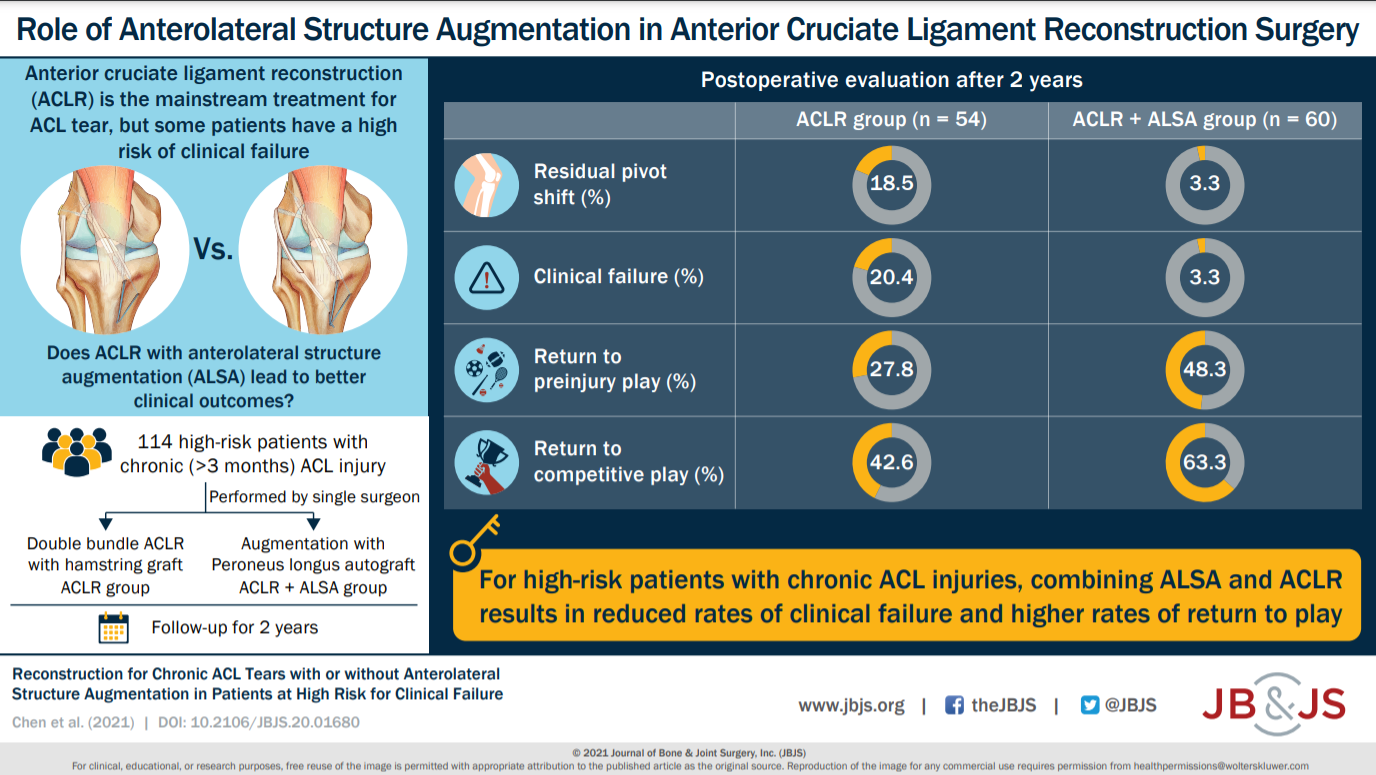
Compared with isolated ACLR, combined ACLR and ALSA resulted in a reduction in persistent rotatory laxity and higher rates of return to preinjury and competitive
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 14 subspecialties. Click here for a
OrthoBuzz has been following the development of the Bridge-Enhanced ACL Repair (BEAR) implant—a synthetic alternative to graft-based anterior cruciate ligament reconstruction—since 2015 (see previous OrthoBuzz
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a
For the last 6 years, JBJS has participated in an “article exchange” collaboration with the Journal of Orthopaedic & Sports Physical Therapy (JOSPT) to support multidisciplinary integration, continuity of care, and
For the last 6 years, JBJS has participated in an “article exchange” collaboration with the Journal of Orthopaedic & Sports Physical Therapy (JOSPT) to support multidisciplinary integration, continuity of
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a

