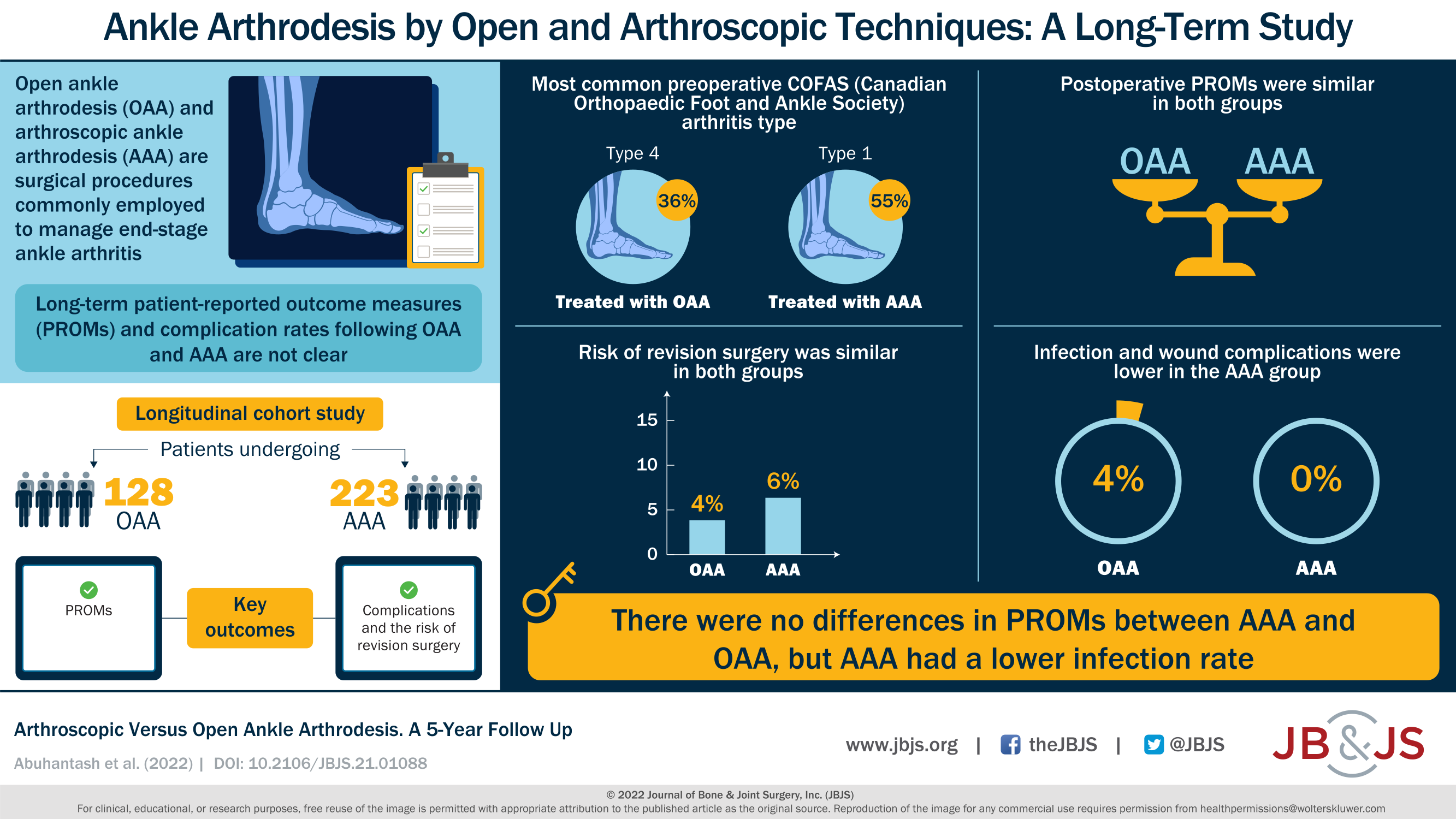
A new JBJS report compares arthroscopic versus open ankle arthrodesis. The authors analyzed long-term patient-reported outcomes, major complications, and reoperations. JBJS Editor-in-Chief Dr. Marc Swiontkowski
Tag: arthroscopy

A new study evaluates trends in knee arthroscopy. Have evidence-based recommendations influenced real-world practice? This post comes from research resident Derek T. Schloemann, MD,
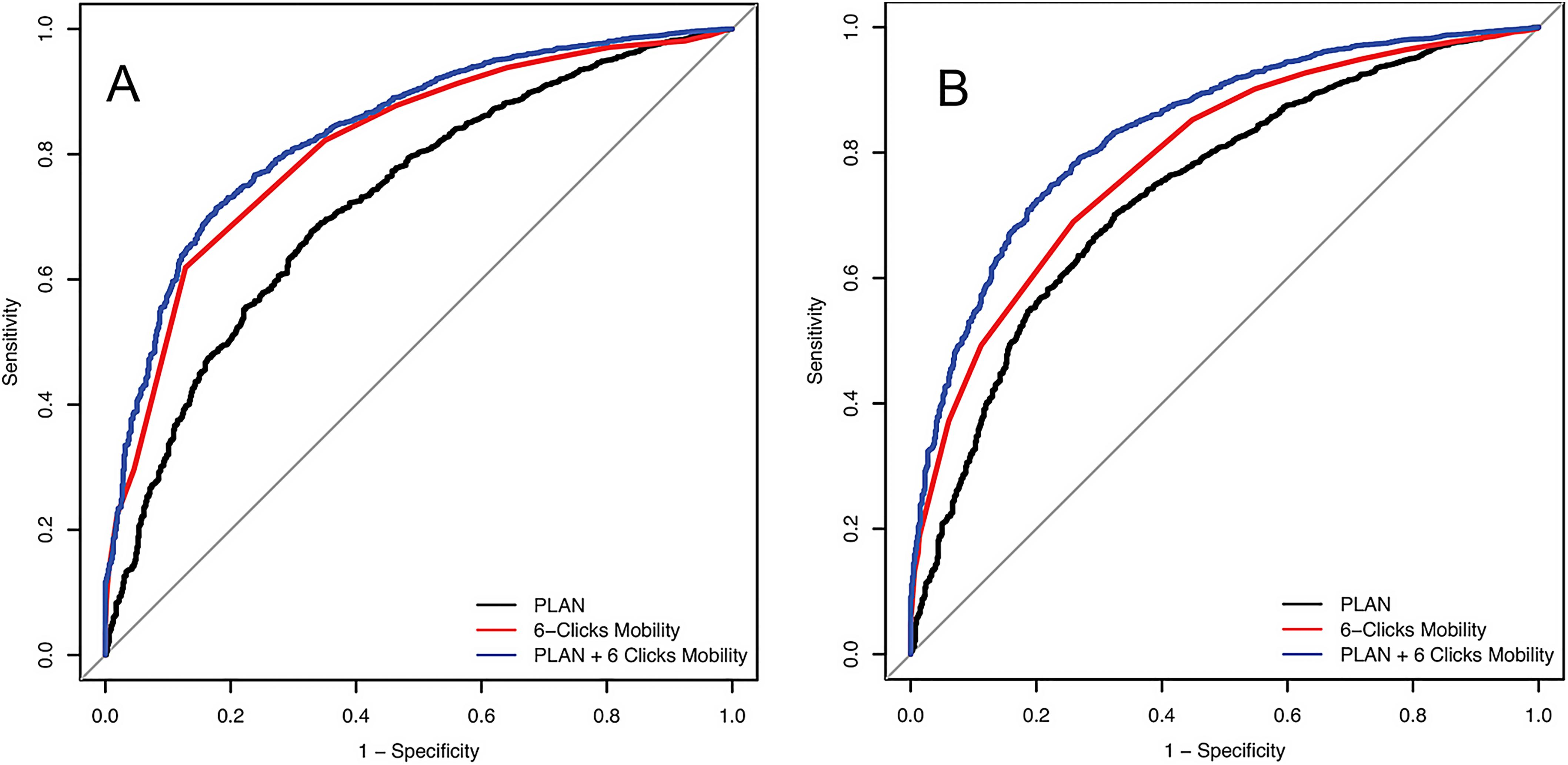
Improving Our Ability to Predict Discharge Disposition After Primary Total Hip and Knee Arthroplasty
The majority of patients who undergo primary total hip arthroplasty (THA) and total knee arthroplasty (TKA) are discharged to home postoperatively, but for some patients,
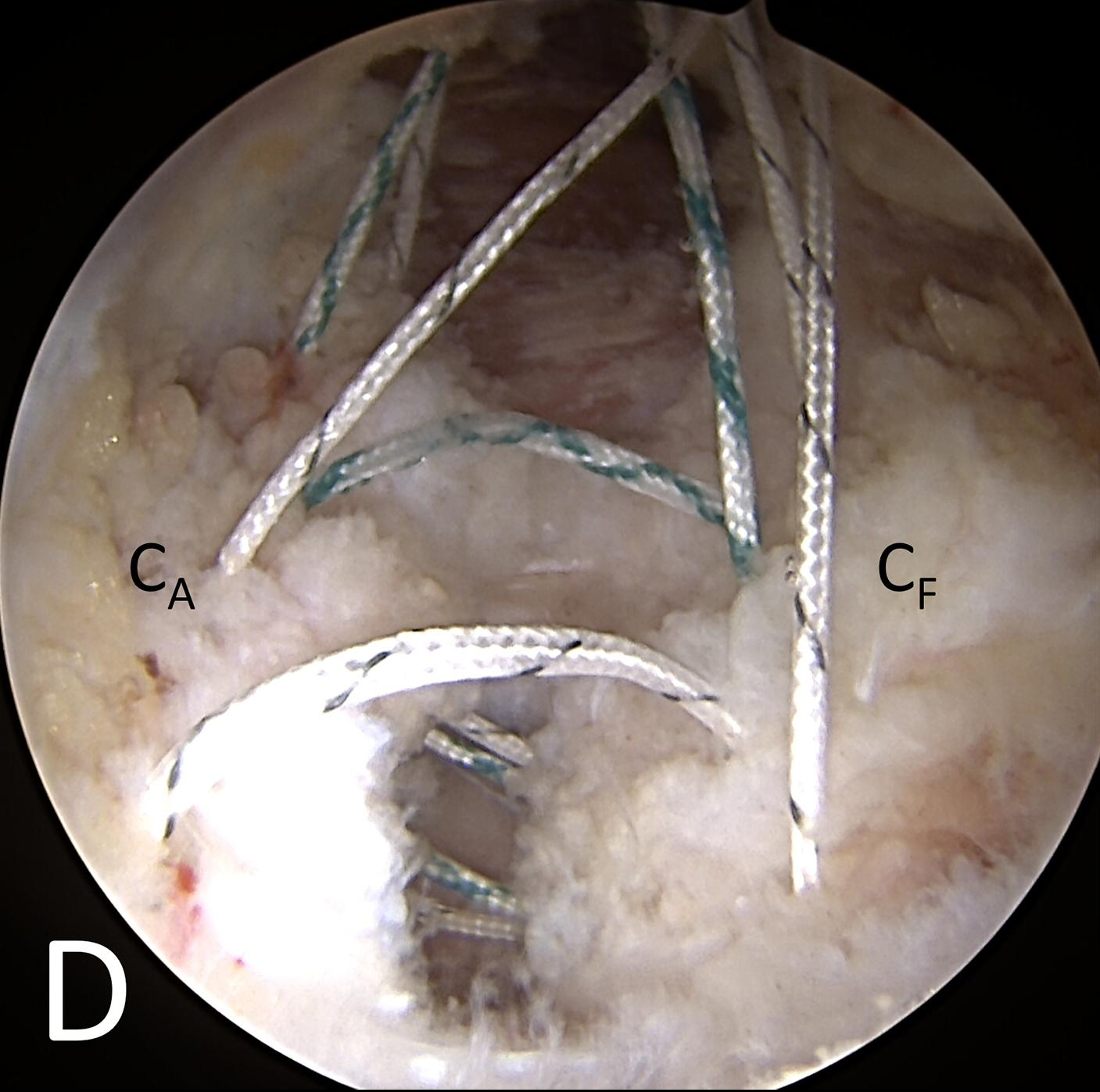
Early hip arthroscopists routinely performed capsulectomies to obtain adequate visualization within the hip joint. As our techniques and skills have evolved, more modern capsulotomies are
The performance of orthopaedic procedures in ambulatory surgery centers (ASCs) continues to increase in the US. This practice is accelerating for multiple reasons: patients want to sleep in their own beds, hospitals can present a risky environment for
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Frederick A. Matsen, MD and Jeremy S. Somerson, MD. The coronavirus pandemic is
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties.
One goal of an orthopaedic surgery residency is to prepare residents for the procedures they will perform when they are attendings. Yet, until the retrospective
Under one name or another, The Journal of Bone & Joint Surgery has published quality orthopaedic content spanning three centuries. In 1919, our publication was
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click