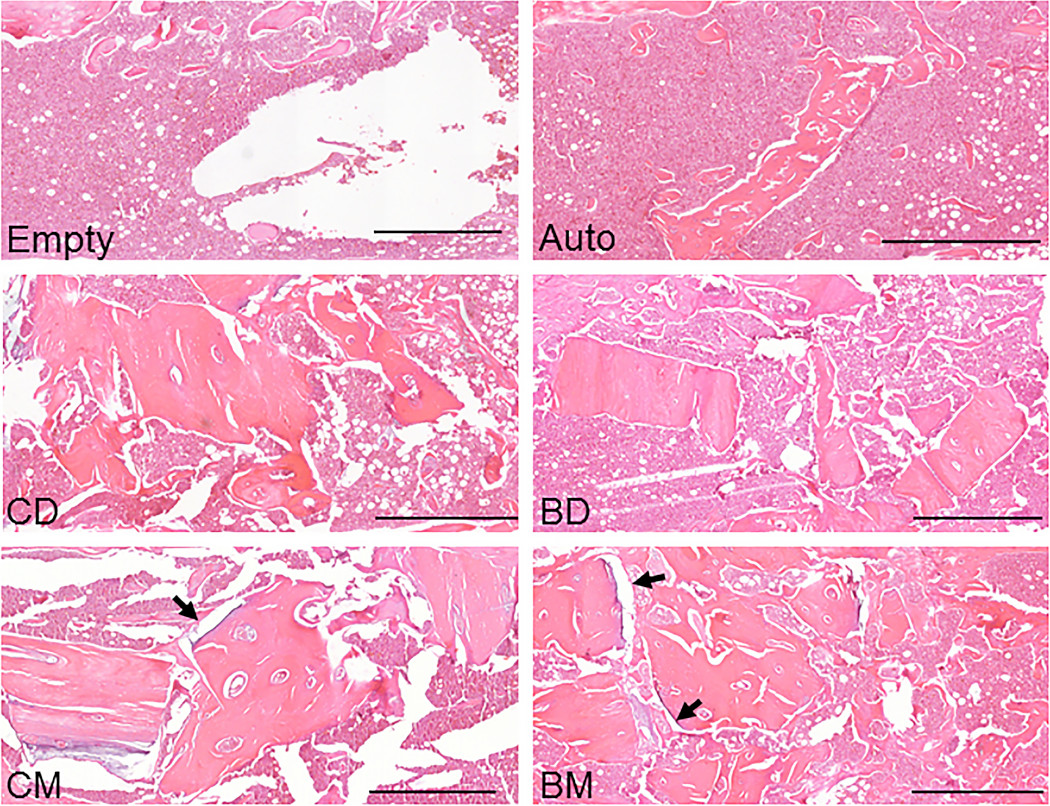
The findings of a new animal study suggest that bisphosphonate treatment in donors may indeed be relevant when mineralized allografts are used in orthopaedic procedures.
Tag: bisphosphonates
The recent JBJS Guest Editorial “What’s New in Osteoporosis and Fragility Fractures” provides an update on this important area of orthopaedic research. The authors review
In the past several years, the orthopaedic community has become highly engaged in improving the follow-up management of patients presenting with fragility fractures. We have
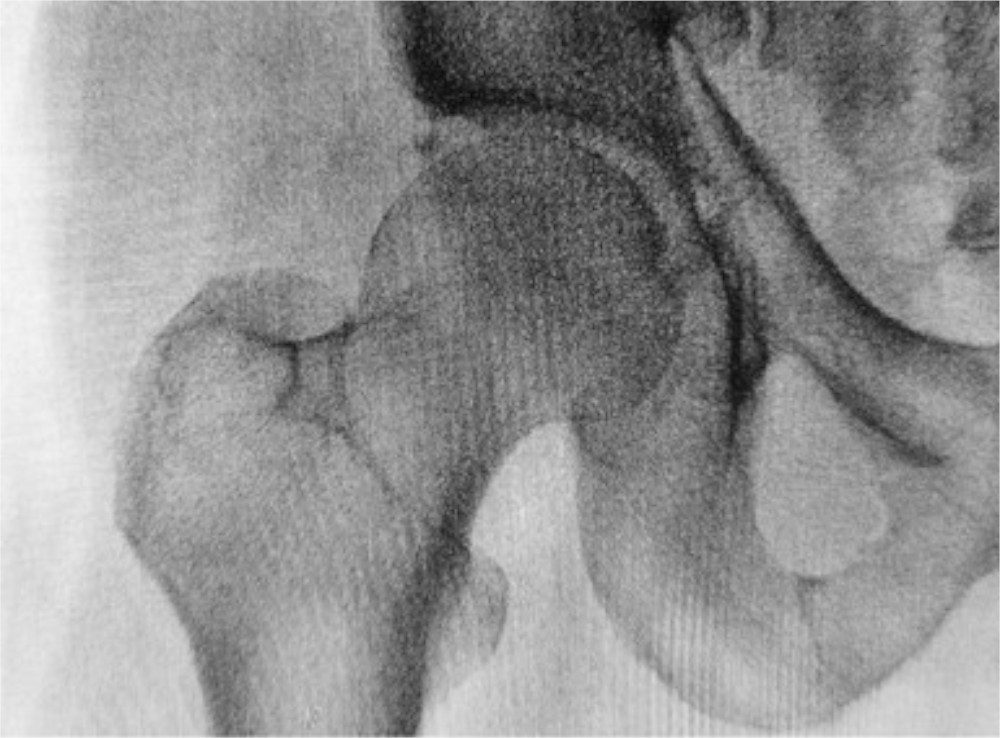
We posted our first “Case Connections” article about bisphosphonate-related atypical femoral fractures (AFFs) one year ago. Since then, JBJS Case Connector has published three additional case reports on
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties.
In December 1996, a group of investigators reported the results of the Fracture Intervention Trial, a randomized controlled trial that compared the effect of alendronate
Physicians worldwide frequently prescribe bisphosphonates such as alendronate (Fosamax) and ibandronate (Boniva) to treat osteoporosis and prevent fragility fractures. Unfortunately, long-term bisphosphonate use has been
A recent study in the Journal of Clinical Endocrinology & Metabolism found that approximately one out of 200 Taiwanese who used oral alendronate long term