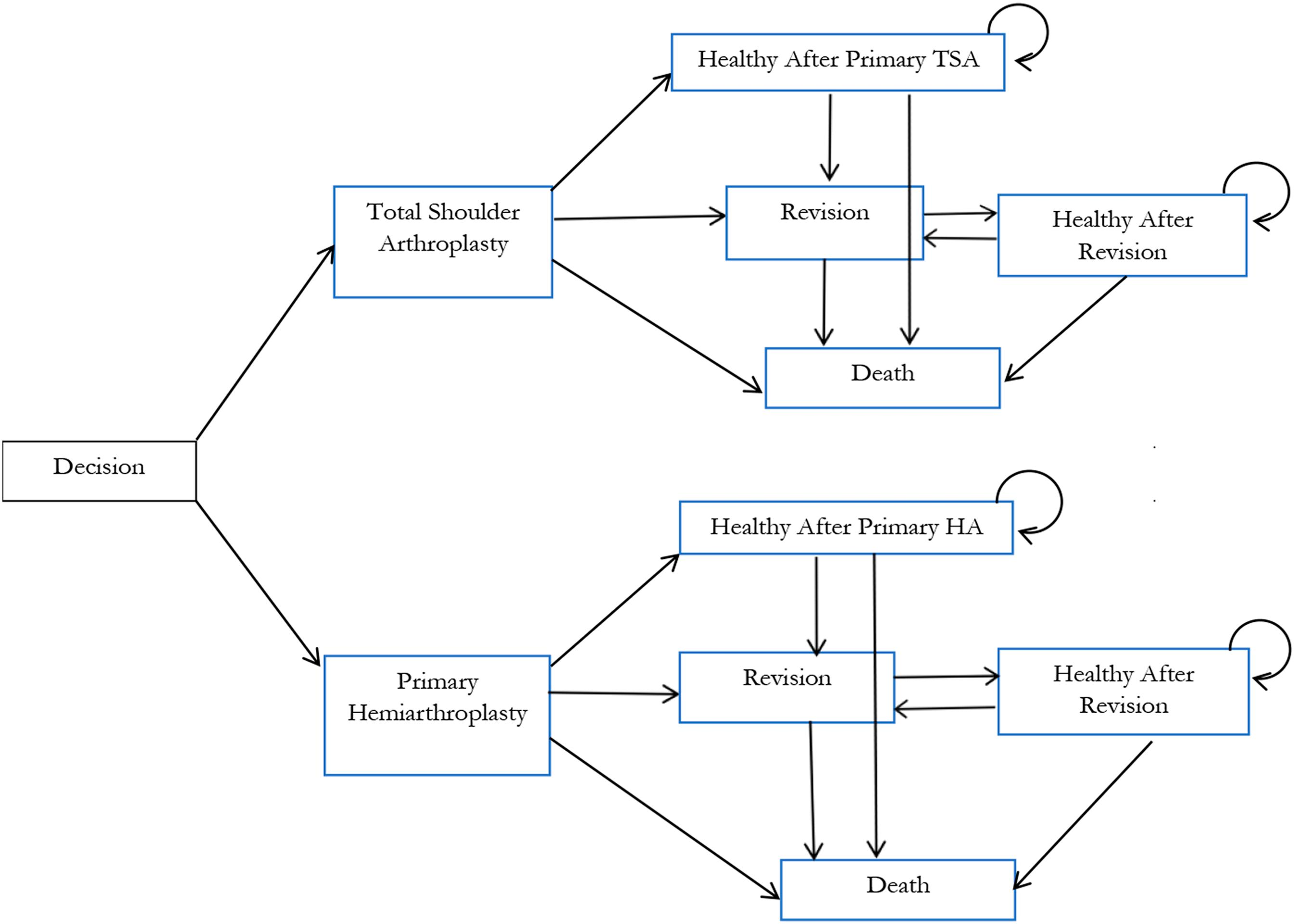
In a new study reported in JBJS, Lapner et al. conducted a cost-utility analysis of total shoulder arthroplasty (TSA) versus hemiarthroplasty from the perspective of Canada’s publicly funded health-care system. They used
Tag: cost effectiveness
The cost-effectiveness analysis of platelet-rich plasma (PRP) for knee osteoarthritis by Rajan et al. in the September 16, 2020 issue of JBJS is accompanied by
The two numbers that you’ll want to remember from the computer model-based cost-effectiveness study by McLawhorn et al. in the January 20, 2016 Journal of