Recent studies on periprosthetic joint infection (PJI) and other topics are presented in the JBJS Guest Editorial “What’s New in Musculoskeletal Infection.” Here, we spotlight
Tag: debridement
Recent findings on fracture management and other trauma-related news are presented in the JBJS Guest Editorial “What’s New in Orthopaedic Trauma.” Here, we spotlight the
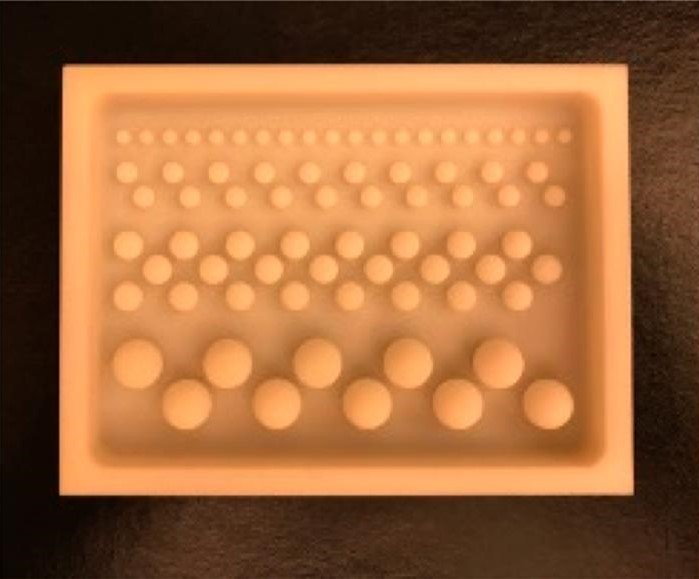
The incorporation of antibiotics within polymethylmethacrylate (PMMA) has been widely used over recent decades for managing infection following skeletal trauma. Early research helped to
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click
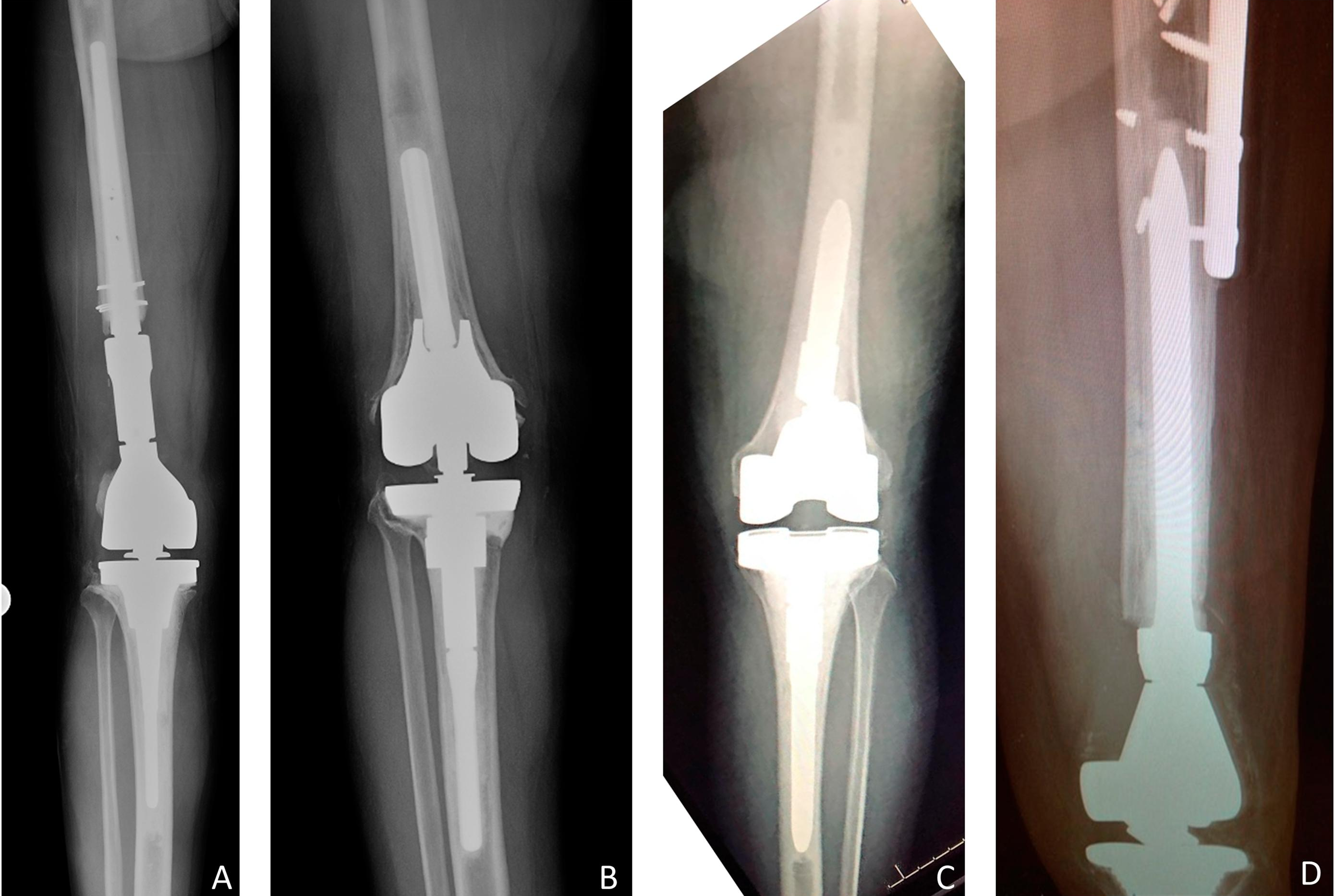
Nowadays, chronic deep periprosthetic joint infections (PJIs) are typically treated with 2-stage exchange arthroplasty, but what about acute PJIs? In the December 6, 2017 edition
This basic science tip comes from Fred Nelson, MD, an orthopaedic surgeon in the Department of Orthopedics at Henry Ford Hospital and a clinical associate
OrthoBuzz regularly brings you a current commentary on a “classic” article from The Journal of Bone & Joint Surgery. These articles have been selected by
Irrigation and debridement of open fractures have been standard practices since the late 1800s. However, the finer details have not been agreed upon. For example,