Recent findings on fracture management and other trauma-related news are presented in the JBJS Guest Editorial “What’s New in Orthopaedic Trauma.” Here, we spotlight the
Tag: external fixation
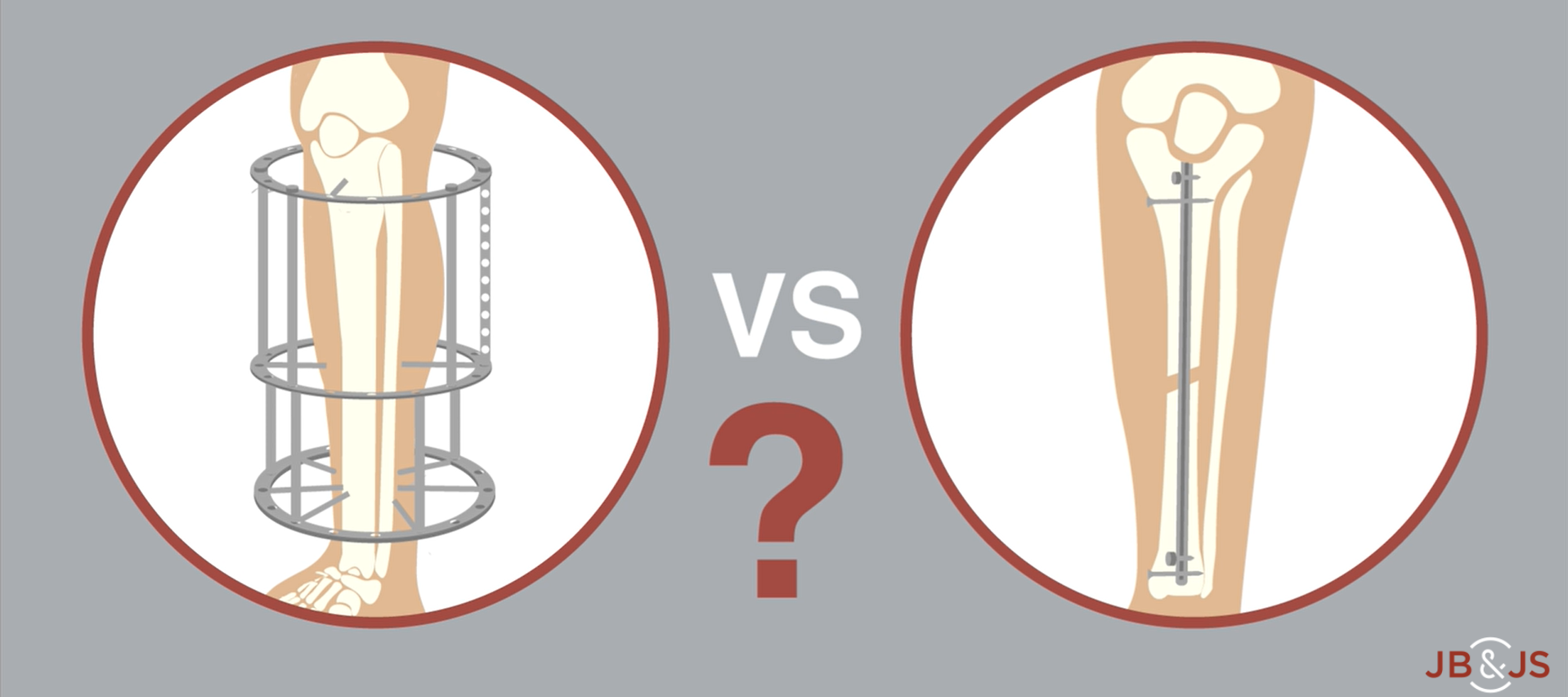
A new RCT provides Level I evidence for internal vs. external fixation of severe open tibial fractures. High-level data have been lacking until now. In
Mechanical factors undoubtedly play a role in the rate and quality of fracture healing. For example, the seminal work on fracture strain by the late
Generally speaking, orthopaedic surgeons in low-resourced environments deliver the best care for their patients with skill, creativity, and passion. These surgeons are accustomed to scrambling
This post comes from Fred Nelson, MD, an orthopaedic surgeon in the Department of Orthopedics at Henry Ford Hospital and a clinical associate professor at
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties.