Recent findings on fracture management and other trauma-related news are presented in the JBJS Guest Editorial “What’s New in Orthopaedic Trauma.” Here, we spotlight the
Tag: fractures
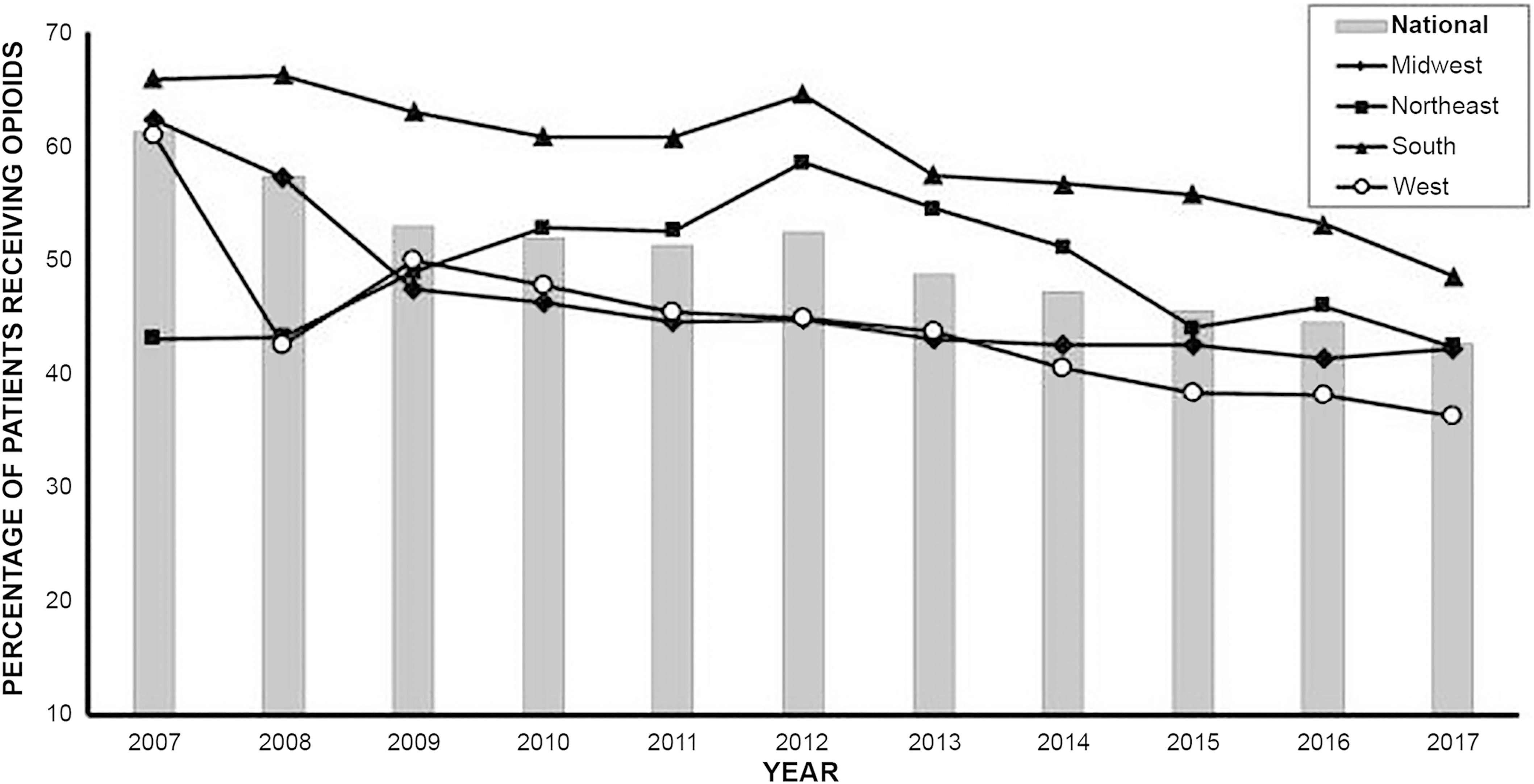
The opioid crisis in America has been well documented. The CDC reports that estimated deaths from drug overdoses topped 100,000 in 2021. Estimated deaths involving
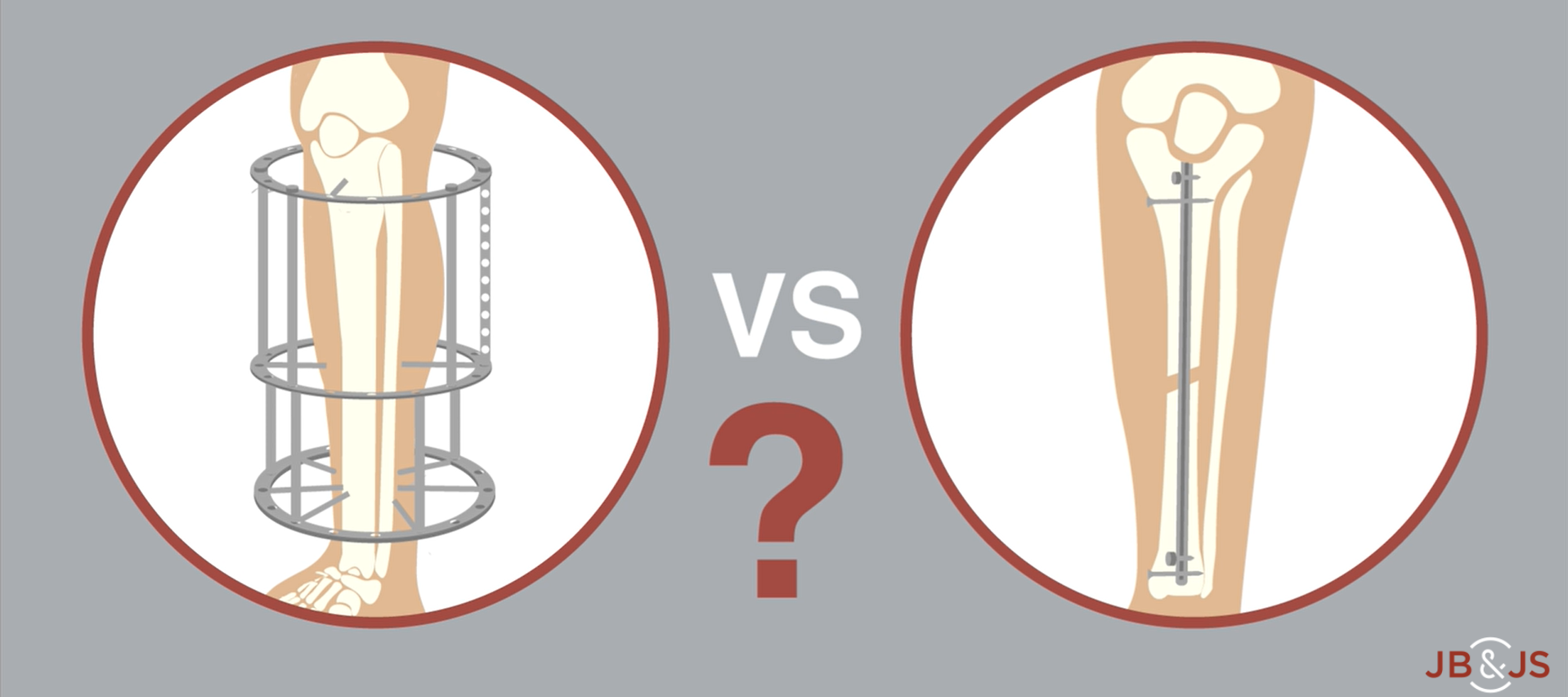
A new RCT provides Level I evidence for internal vs. external fixation of severe open tibial fractures. High-level data have been lacking until now. In
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Brett A. Freedman, MD, in response to a study published in JAMA about a
Each month during the coming year, OrthoBuzz will bring you a current commentary on a “classic” article from The Journal of Bone & Joint Surgery. These articles
Pelvic binders can provide lifesaving compression in patients with hemodynamically unstable pelvic injuries. But a report in the March 11, 2015 JBJS Case Connector by
In last month’s Editor’s Choice, JBJS Editor in Chief Vern Tolo. MD, called for more concerted efforts among orthopaedists to link care of fragility fractures
The article “Declining Rates of Osteoporosis Management Following Fragility Fractures in the U.S., 2000 through 2009” by Balasubramanian, et al. in the April 2, 2014