The recent JBJS Guest Editorial “What’s New in Osteoporosis and Fragility Fractures” provides an update on this important area of orthopaedic research. The authors review
Tag: fragility fracture
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from James Blair, MD, in response to a recent edition of the OrthoJOE podcast. Geriatric
Osteoporosis is the major contributor to the increasing incidence of fragility fractures associated with low-energy falls. The other contributor is the populous baby-boomer generation that
“We believe that bone health screening should be considered in all orthopaedic surgical candidates who are ≥50 years of age.” So proclaim Kadri et al.,
The orthopaedic community began to move away from individual fracture classifications in the mid-1980s. The basis for that shift was the need for wider recognition
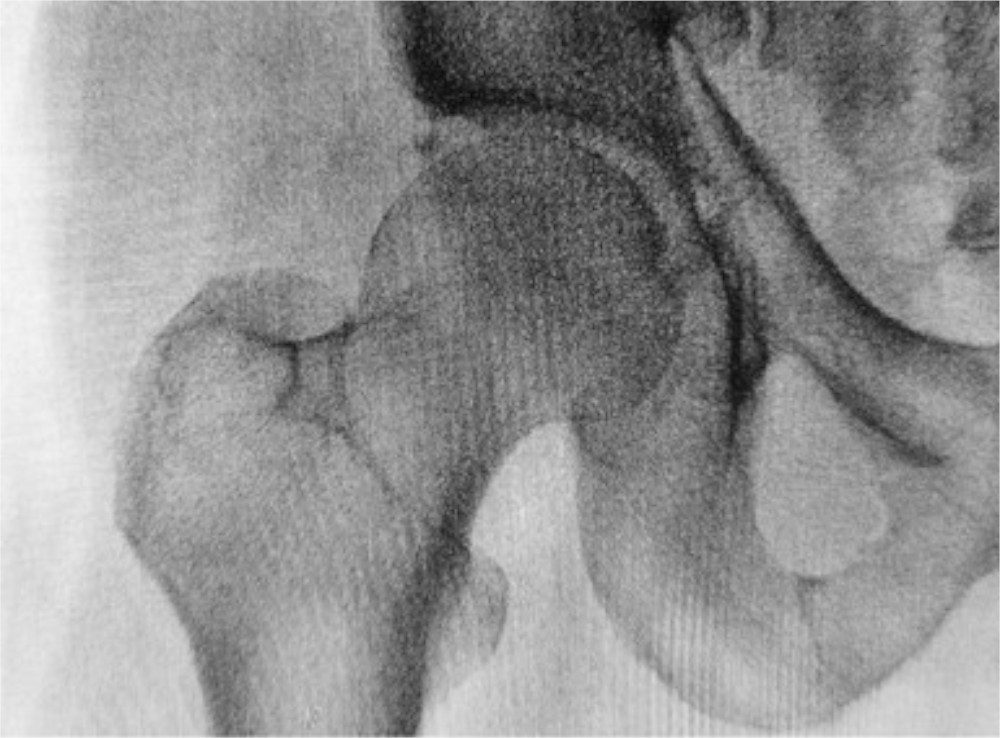
Osteoporosis is a “silent” disease, often becoming apparent only after a patient older than 50 sustains a low-energy fracture of the wrist, proximal humerus, or
Fracture liaison services and similar coordinated, multidisciplinary fragility-fracture reduction programs for patients with osteoporosis work (see related OrthoBuzz posts), but until now, the data corroborating
Orthopaedic care teams can play an active role in evaluating and optimizing their patients’ bone health to help prevent primary and secondary fragility fractures and
On Thursday evening, June 28 and all day Friday, June 29 in Boston, The American Orthopaedic Association (AOA) and the National Association of Orthopaedic Nurses
How well do fracture liaison services (FLSs) work in terms of patients who’ve had a fragility fracture receiving a recommendation for anti-osteoporosis treatment? Very well,