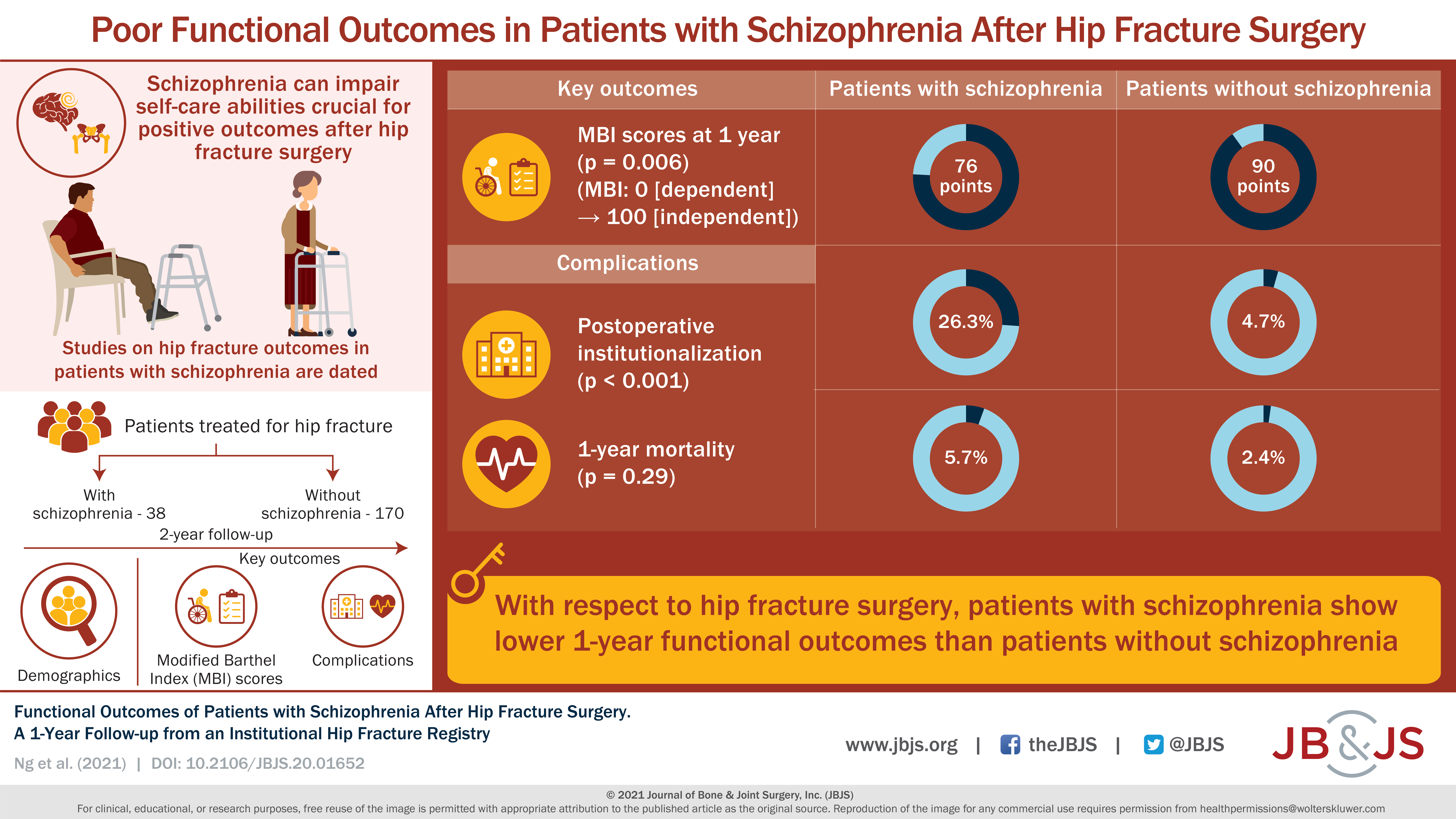
Thirty-eight patients with schizophrenia were compared with 170 geriatric patients without schizophrenia who underwent a surgical procedure for a hip fracture. Read the full article
Tag: Hip
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 14 subspecialties. Click here for a
Full article Background: Current guidelines recommend serum erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) as the first-line testing for evaluation of suspected periprosthetic
There have been concerns that the antifibrinolytic drug tranexamic acid (TXA) might increase the postoperative risk of cardiovascular events. Our objective was to determine whether
The purpose of this study was to estimate the incidence of reoperation and the effect of implant position on the risk of reoperation within 12
Total hip arthroplasty (THA) is an effective operation for the management of end-stage hip osteoarthritis, but long-term success can be limited by wear of the
Prescription opioid use is epidemic in the U.S. Recently, an association was demonstrated between preoperative opioid use and increased health-care utilization following abdominal surgeries. #JBJSInfographics
Obesity is a negative prognostic factor for various surgical procedures. https://bit.ly/2JKUj4C #JBJSInfographics #VisualAbstract
For elderly trauma patients, a basic goal is early mobilization, as immobilization can trigger various complications, such as venous thromboembolism, pneumonia, urinary tract infections, and
Morbidly obese patients with severe osteoarthritis benefit from successful total joint arthroplasty. However, morbid obesity increases the risk of complications. https://bit.ly/2qpfj8w #JBJS