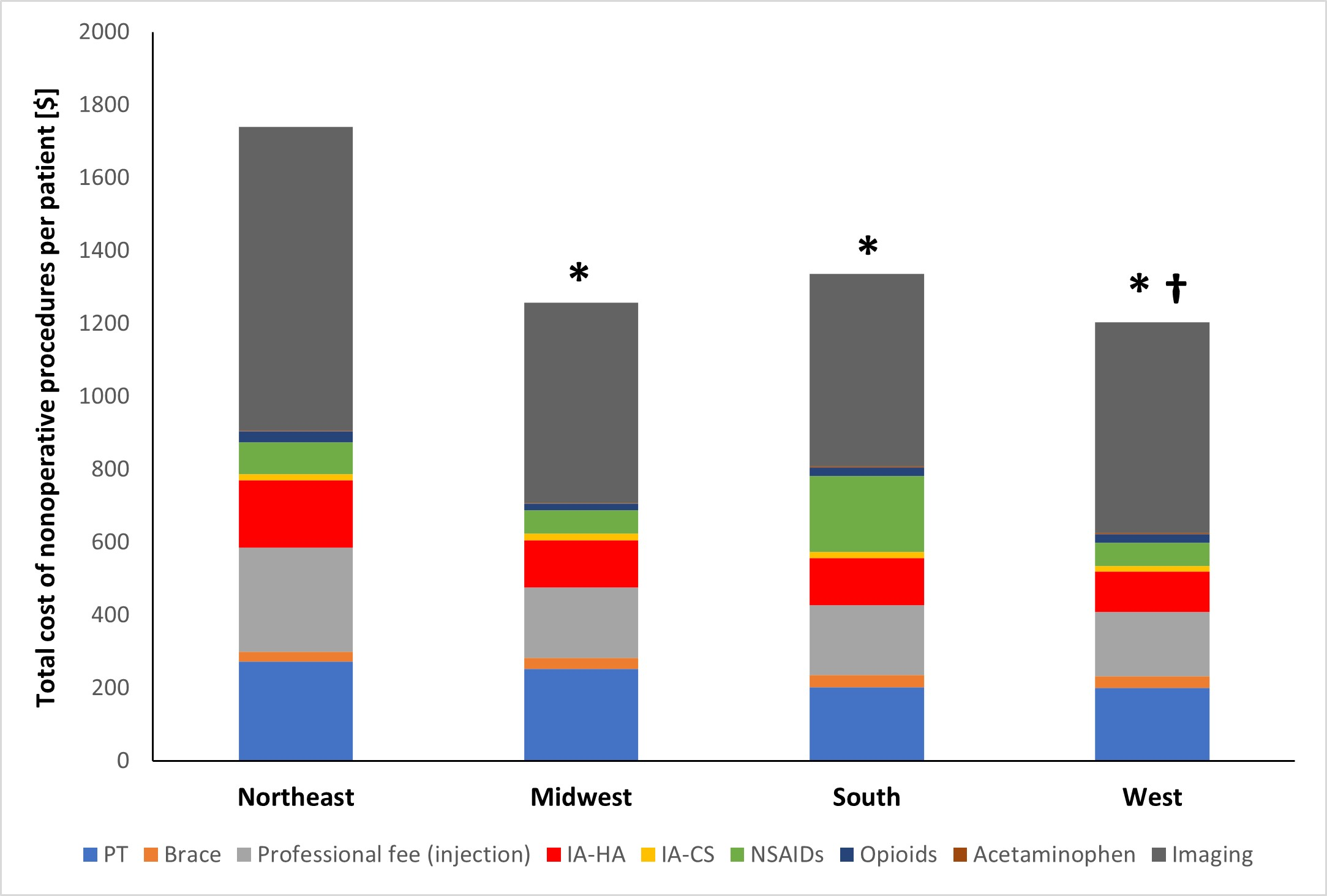
A new JBJS study reviews costs associated with nonoperative management of osteoarthritis in the 1-year period leading up to total knee arthroplasty (TKA). JBJS Deputy
Tag: hyaluronic acid

Intra-articular hyaluronic acid injections, also known as viscosupplementation, are a common treatment option for many patients with end-stage osteoarthritis of the knee. However, the effectiveness
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Prof. Joerg Jerosch, in response to a recent article in JBJS Reviews. I congratulate Vannabouathong
In a recent OrthoBuzz post, I commented on the apparent benefits to patients when Scottish hip-fracture guidelines were followed. Now, in a “closer-to-home” study in
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click
Orthopaedists frequently treat knee osteoarthritis with hyaluronic acid (HA) or corticosteroid injections, but which works better? The 99 patients in a double-blinded randomized controlled trial
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties.
A “Clinical Therapeutics” article in the March 12, 2015 New England Journal of Medicine focuses on viscosupplementation for knee osteoarthritis (OA). In presenting a case
We stumbled upon three recent studies of knee osteoarthritis (OA) that shed interesting new light on a condition that all orthopaedists deal with. –A “network”