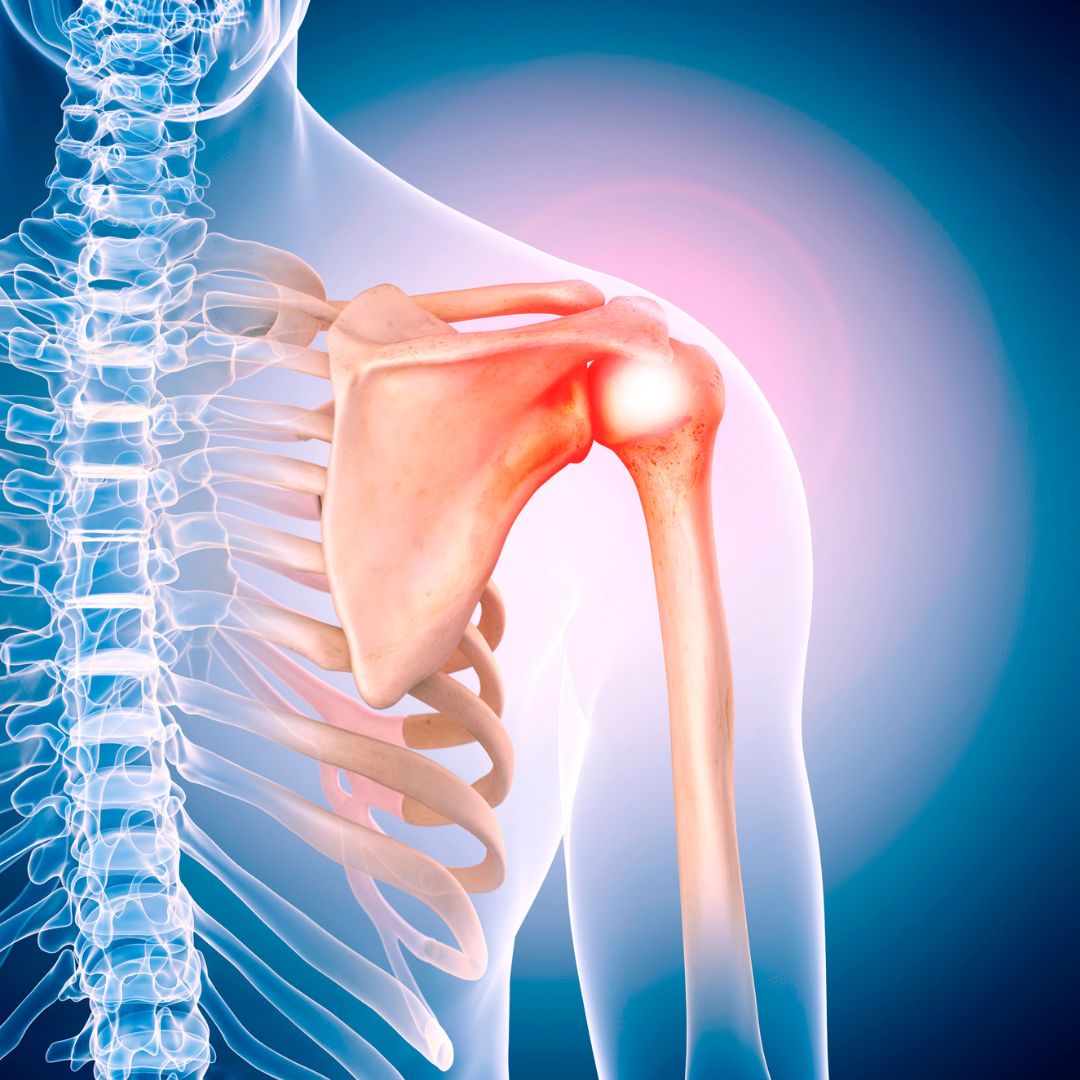
Rotator cuff repair, shoulder arthroplasty, shoulder instability, and the treatment of elbow injuries are among the topics of recent studies reviewed in the new JBJS
Tag: Infection

OrthoBuzz readers who’d like to learn more about the Major Extremity Trauma and Rehabilitation Consortium (METRC) are encouraged to check out the recent episode of
Recent findings on fracture management and other trauma-related news are presented in the JBJS Guest Editorial “What’s New in Orthopaedic Trauma.” Here, we spotlight the
In a study now reported in JBJS, Acuña et al. analyzed Medicare reimbursements associated with revision total hip arthroplasty (THA) procedures. After adjusting for inflation, they found that the mean
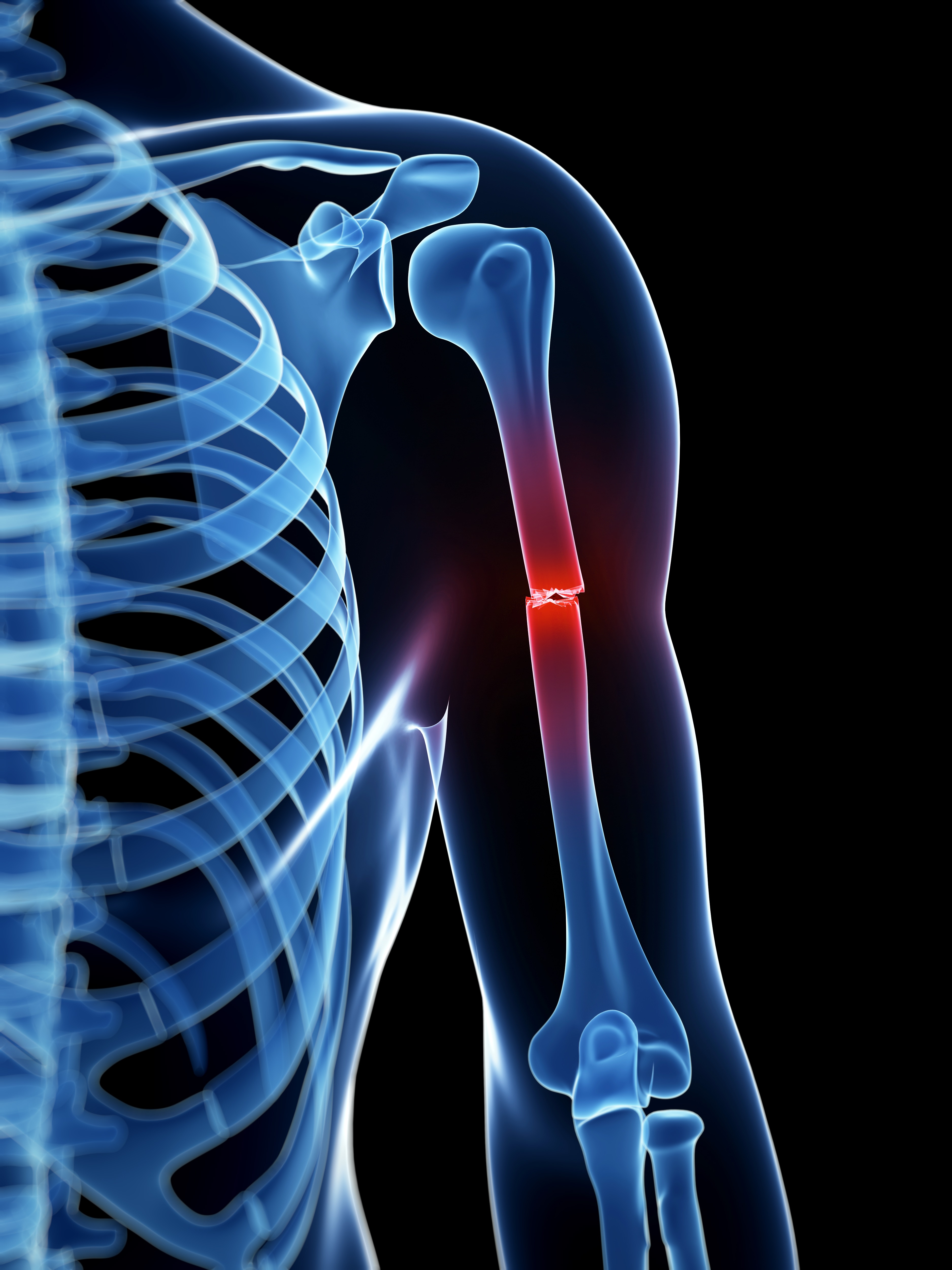
Infection after surgery to treat a tibial shaft fracture can have devastating consequences, with significant associated costs and burdens. Although research has identified general risk
Surgeons performing revision shoulder arthroplasty typically order postoperative antibiotics to be administered while they wait for results from intraoperative cultures. Based on their index of
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a
Prosthetic infections involving total hip or knee implants are bad enough, but infections involving pelvic endoprostheses following tumor resection can be particularly devastating, often necessitating
An elevated International Normalized Ratio (INR)—a standardized gauge for how long it takes blood to clot—is rarely a good sign when someone is about to