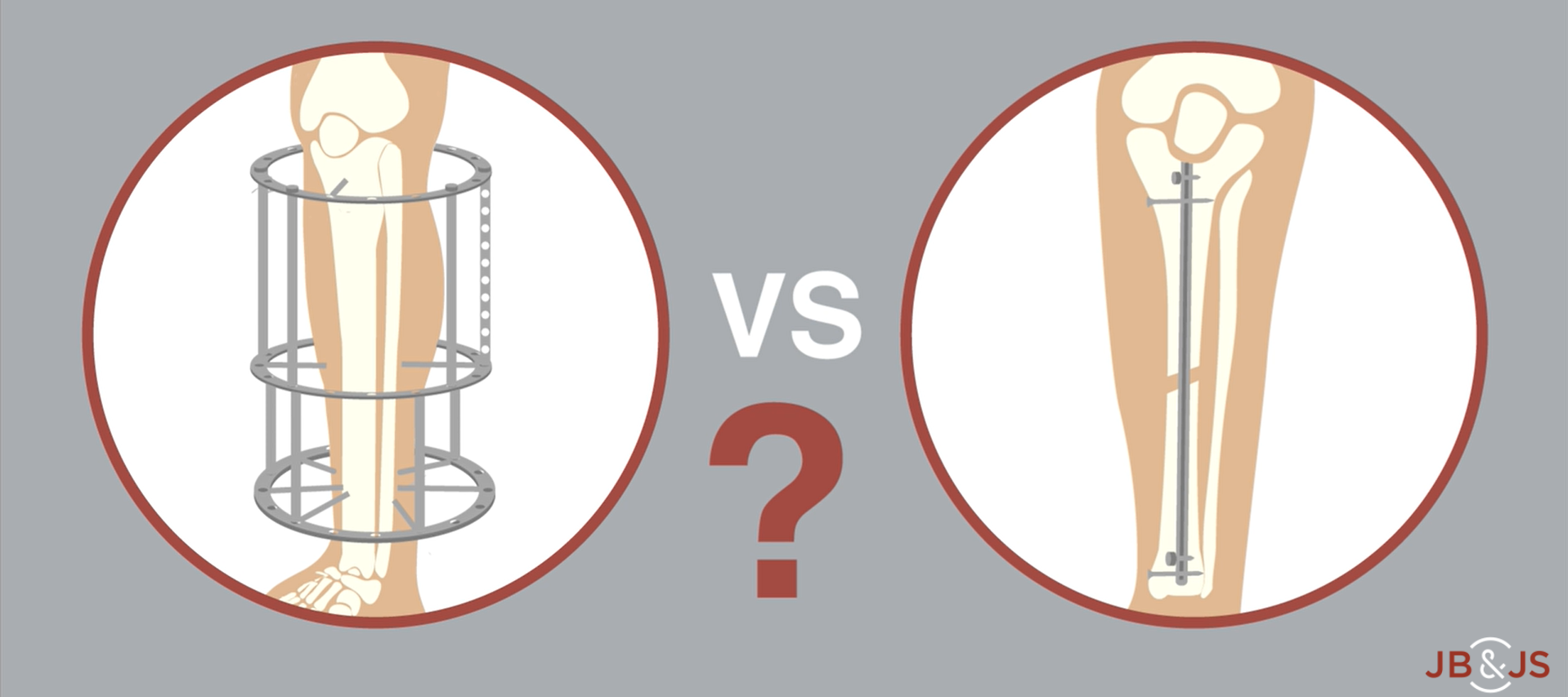
A new RCT provides Level I evidence for internal vs. external fixation of severe open tibial fractures. High-level data have been lacking until now. In
Tag: internal fixation
Notice of Retraction: March 2, 2022 We regret to inform you that The Journal of Bone and Joint Surgery must retract the article entitled “Ankle
According to the orthopaedic literature, the risk of vascular injury during internal fixation of a proximal femoral fracture is low. But applying the findings from
Each month during the coming year, OrthoBuzz will bring you a current commentary on a “classic” article from The Journal of Bone & Joint Surgery. These articles