Recent studies on periprosthetic joint infection (PJI) and other topics are presented in the JBJS Guest Editorial “What’s New in Musculoskeletal Infection.” Here, we spotlight
Tag: Irrigation and Debridement
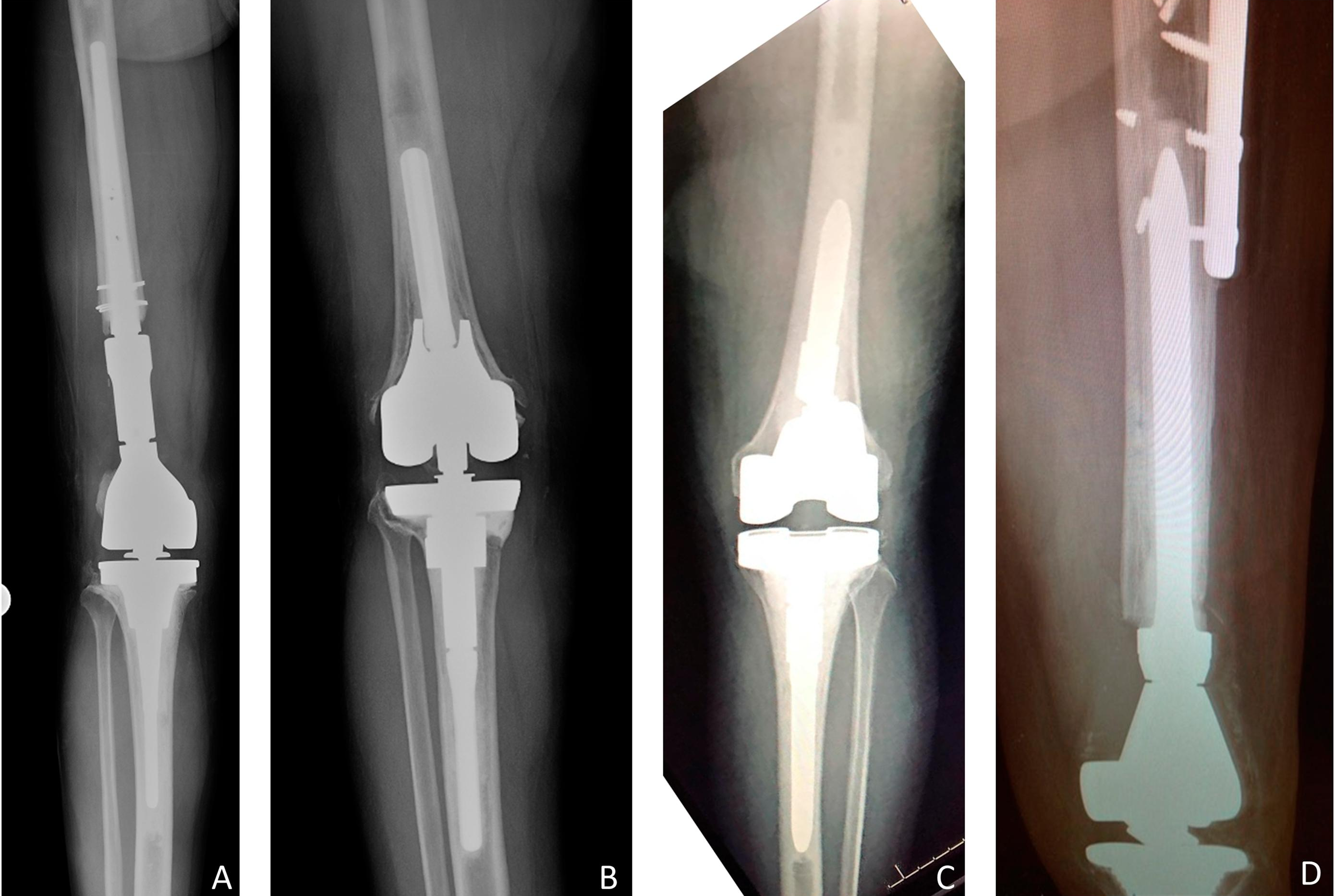
It’s hard to contemplate “conservative treatment” in the case of a revised total knee arthroplasty (rTKA) with extensive instrumentation that needs a reoperation due to
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for
Orthopaedic surgeons have developed a heightened awareness of the scientific evidence that supports the decisions that they make in the care of patients. Levels of