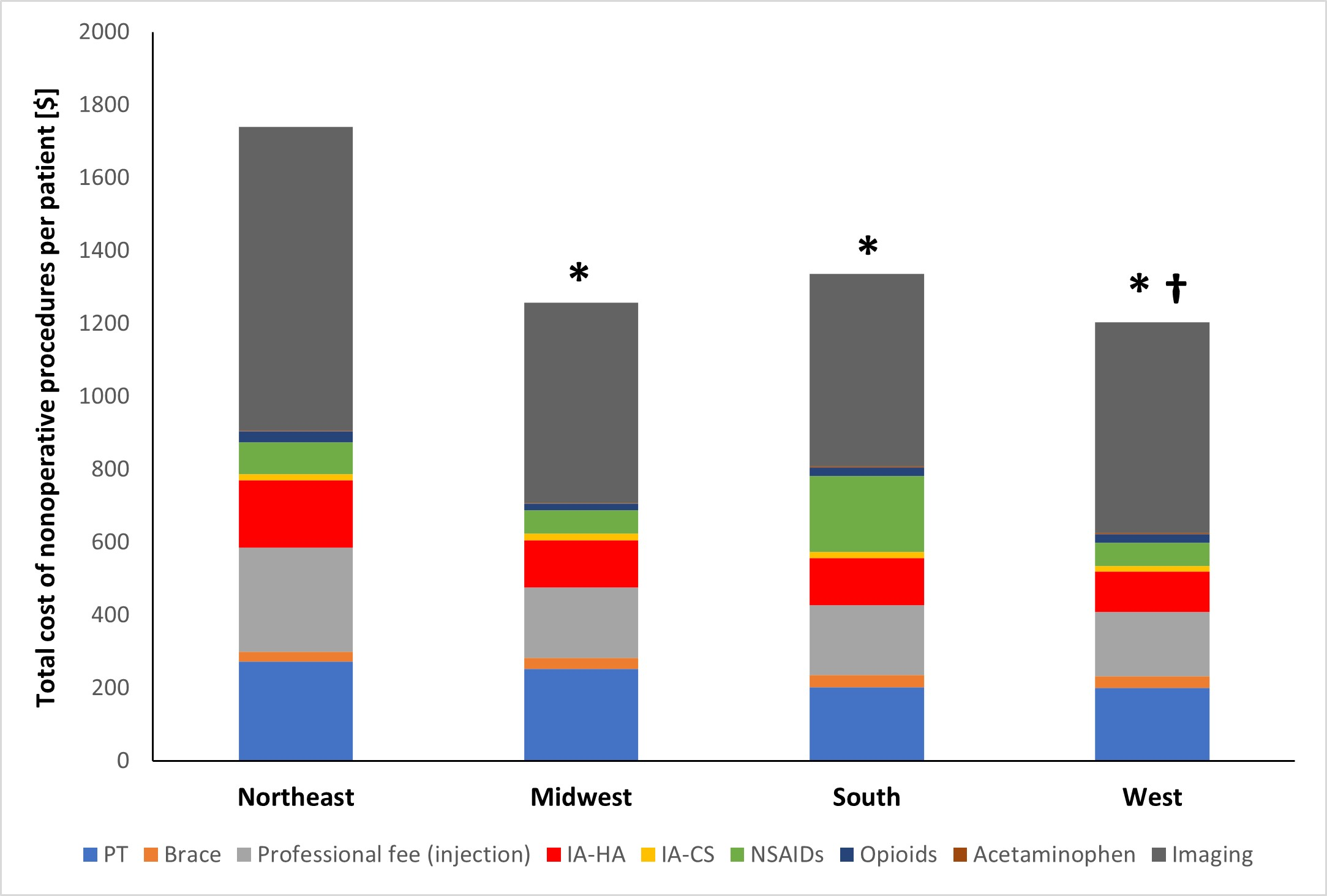
A new JBJS study reviews costs associated with nonoperative management of osteoarthritis in the 1-year period leading up to total knee arthroplasty (TKA). JBJS Deputy
Tag: knee arthritis
The orthopaedic community worldwide—and especially those of us in the US, the nation most notorious for over-prescribing—has become very cognizant of the epidemic of opioid
Sport activity continues to increase in priority in modern society. And with a concomitant increase in single-sport focus early in life and near year-round training,
Attempts by orthopaedists to repair torn human ACLs have failed for the most part, so surgeons now rely almost exclusively on removing the torn ligament