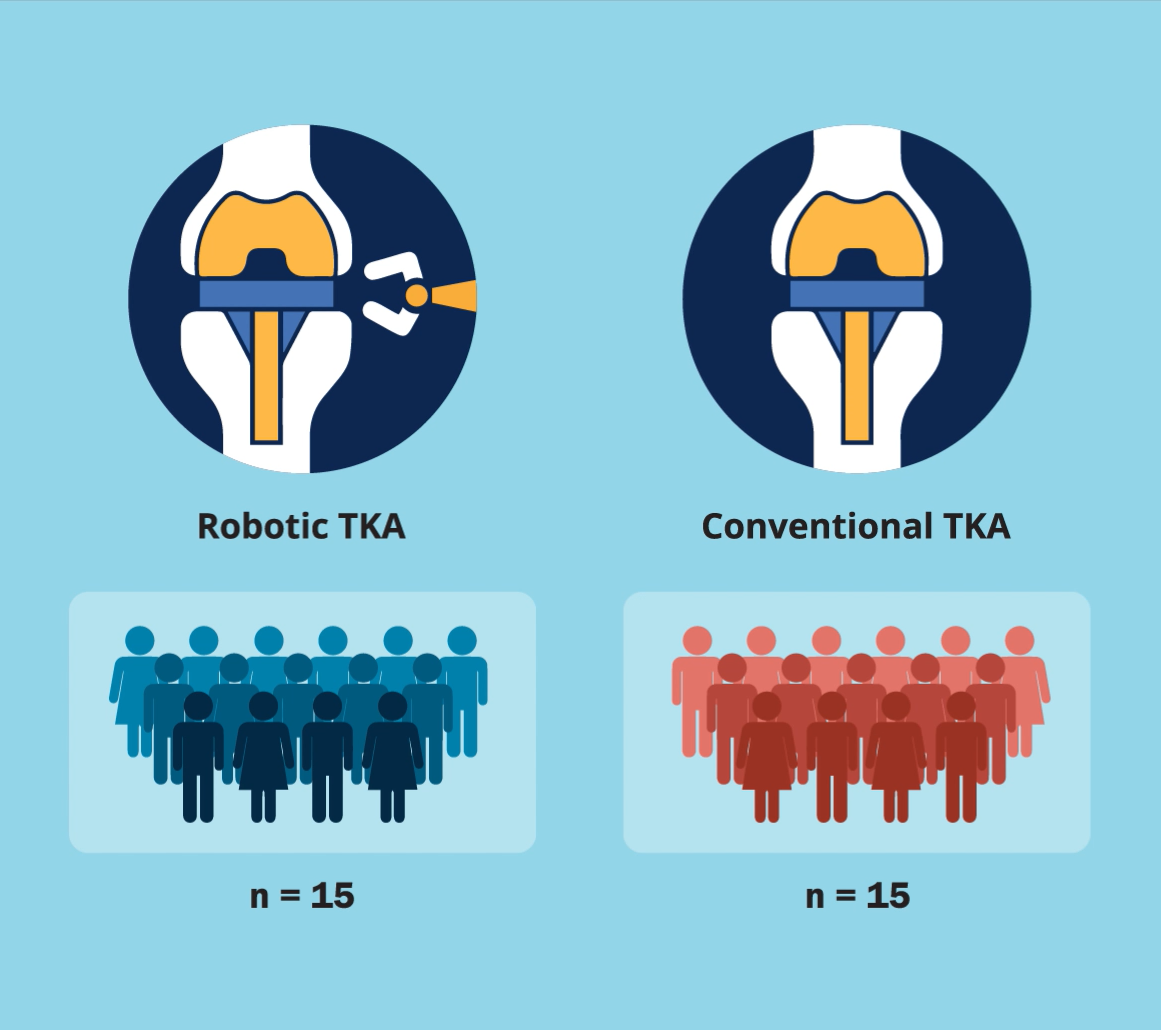
A new JBJS study by Fontalis et al. compares the inflammatory response in robotic-arm-assisted total knee arthroplasty (TKA) vs. conventional jig-based TKA. The investigators also
Tag: knee osteoarthritis
This post comes from Fred Nelson, MD, an orthopaedic surgeon in the Department of Orthopedics at Henry Ford Hospital and a clinical associate professor at
This post comes from Fred Nelson, MD, an orthopaedic surgeon in the Department of Orthopedics at Henry Ford Hospital and a clinical associate professor at
Medial opening-wedge high tibial osteotomy (MOHTO) is a tried-and-true joint preservation technique for medial compartment knee osteoarthritis with varus alignment. Multiple studies have shown good
For the last 6 years, JBJS has participated in an “article exchange” collaboration with the Journal of Orthopaedic & Sports Physical Therapy (JOSPT) to support multidisciplinary integration, continuity of care, and
OrthoBuzz occasionally receives posts from guest bloggers. In response to a recent study in The New England Journal of Medicine, the following commentary comes from Jaime L. Bellamy,
Mark Miller, MD is a professor of orthopaedic surgery at the University of Virginia, founder and co-director of the Miller Review Courses, and former deputy
This post comes from Fred Nelson, MD, an orthopaedic surgeon in the Department of Orthopedics at Henry Ford Hospital and a clinical associate professor at
This post comes from Fred Nelson, MD, an orthopaedic surgeon in the Department of Orthopedics at Henry Ford Hospital and a clinical associate professor at
OrthoBuzz occasionally receives posts from guest bloggers. In response to a recent study in Arthritis Care & Research, the following commentary comes from Jeffrey B. Stambough, MD.