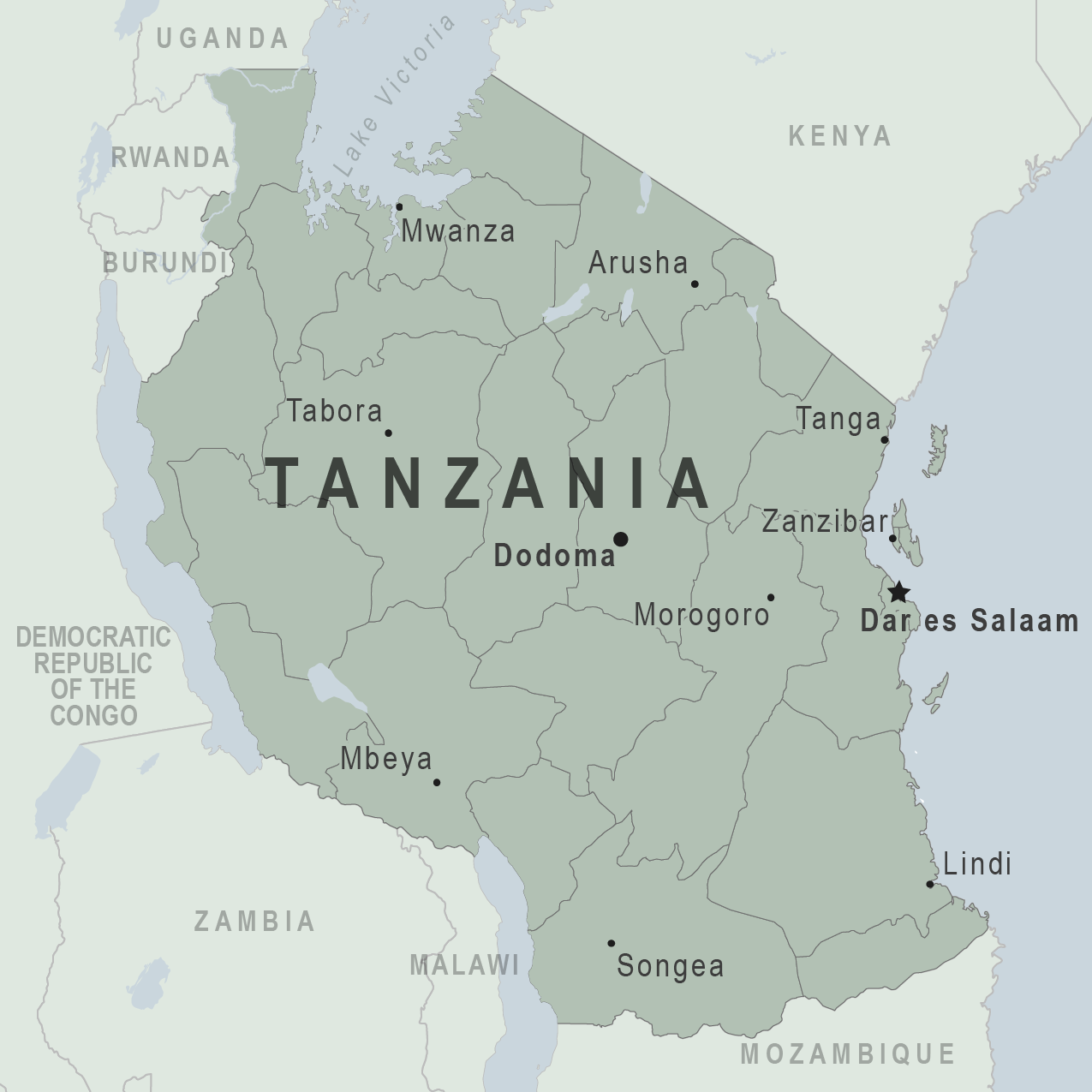
In a recent report in JBJS, Holler et al. investigated risk factors for delayed management of open tibial fractures in Tanzania. As the authors note,
Tag: Open fracture
The prompt administration of prophylactic antibiotics is considered a critical component of open-fracture management. In 2011, the Eastern Association for the Surgery of Trauma (EAST)
Under one name or another, The Journal of Bone & Joint Surgery has published quality orthopaedic content spanning three centuries. In 1919, our publication was
Basic science investigations into clinically relevant orthopaedic conditions are very common—and often very fruitful. What’s not very common is seeing results from large, multicenter randomized
Injuries to the musculoskeletal system are among the most common wounds of war. Compared with extremity injuries in the civilian population, injuries sustained in combat
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties.
Musculoskeletal (MSK) infections are highly prevalent and potentially serious, and orthopaedists are frequently faced with preventing and treating them. Wherever or however they are acquired, these
OrthoBuzz regularly brings you a current commentary on a “classic” article from The Journal of Bone & Joint Surgery. These articles have been selected by
In the November 18, 2015 edition of JBJS, Lawing et al. present a well-documented cohort study comparing the outcomes of open-fracture management with local administration
Irrigation and debridement of open fractures have been standard practices since the late 1800s. However, the finer details have not been agreed upon. For example,