In this post, Deputy Editor for Social Media Dr. Matt Schmitz discusses the new study by Hong et al. in JBJS: “The Effect of Social
Tag: Orthopedics
The long-term effect of distal radial fracture malunion on activity limitations is unknown. https://bit.ly/2qYgOMh #JBJS
Abdel et al. report on the 20-year survivorship of total knee arthroplasty implants that were mechanically aligned (0° ± 3° relative to the mechanical axis)
OrthoBuzz regularly brings you a current commentary on a “classic” article from The Journal of Bone & Joint Surgery. These articles have been selected by the
Surgeons often prescribe more postoperative pain medication than their patients actually use. That’s partly because there is limited procedure-specific evidence-based data regarding optimal amounts and
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Chad Krueger, MD, in response to an Annals of Internal Medicine study investigating
The indications for arthroscopic treatment of musculoskeletal injuries continue to expand as orthopaedists find new and creative ways to apply this flexible technology. The May 2016
Over the past several decades, orthopaedic surgery has enjoyed an explosion in the development of new technologies. These technologies have largely improved the quality of
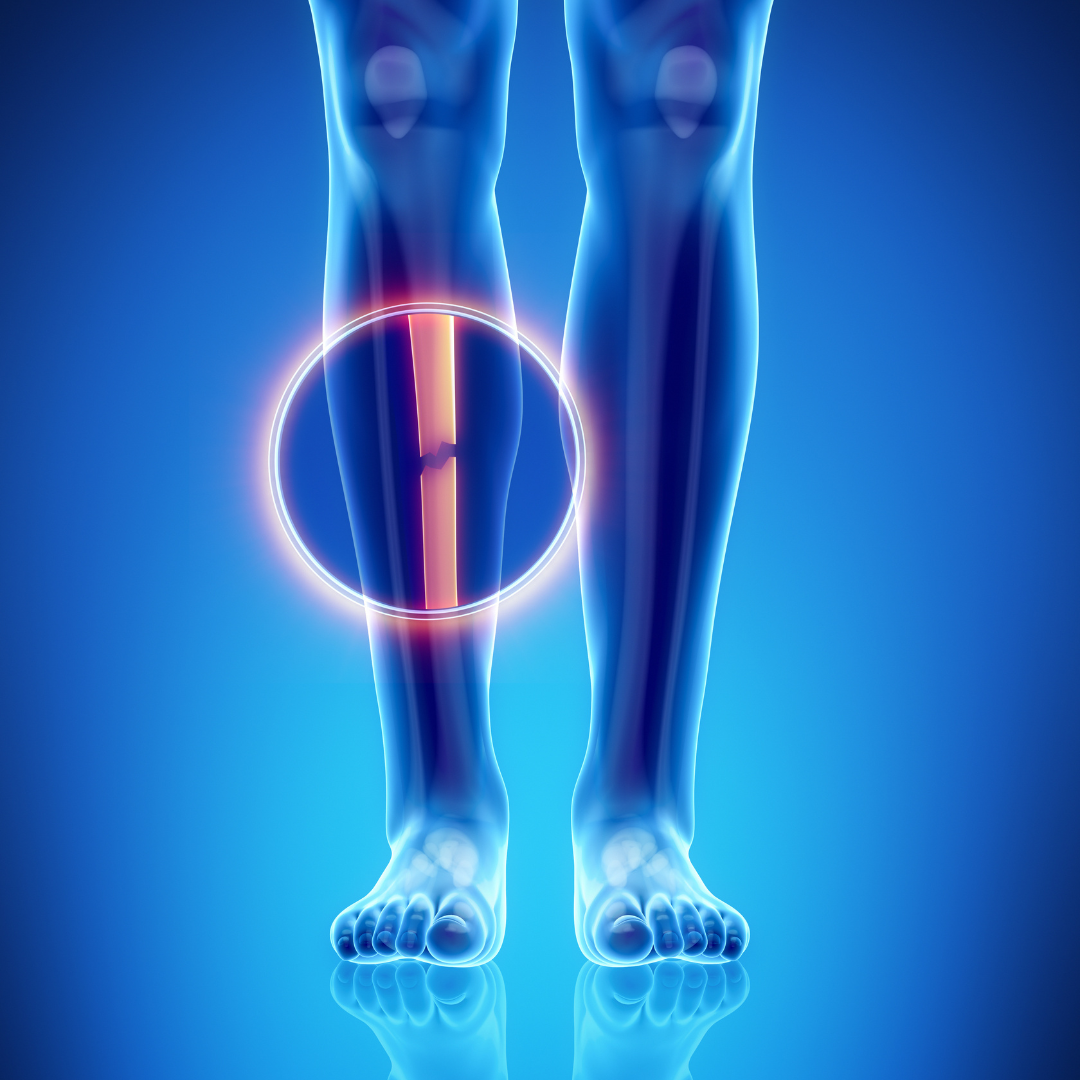
We posted our first “Case Connections” article about bisphosphonate-related atypical femoral fractures (AFFs) one year ago. Since then, JBJS Case Connector has published three additional case reports on
The Centers for Medicare and Medicaid Services (CMS) announced this week that it will not deny claims from providers during the first 12 months of