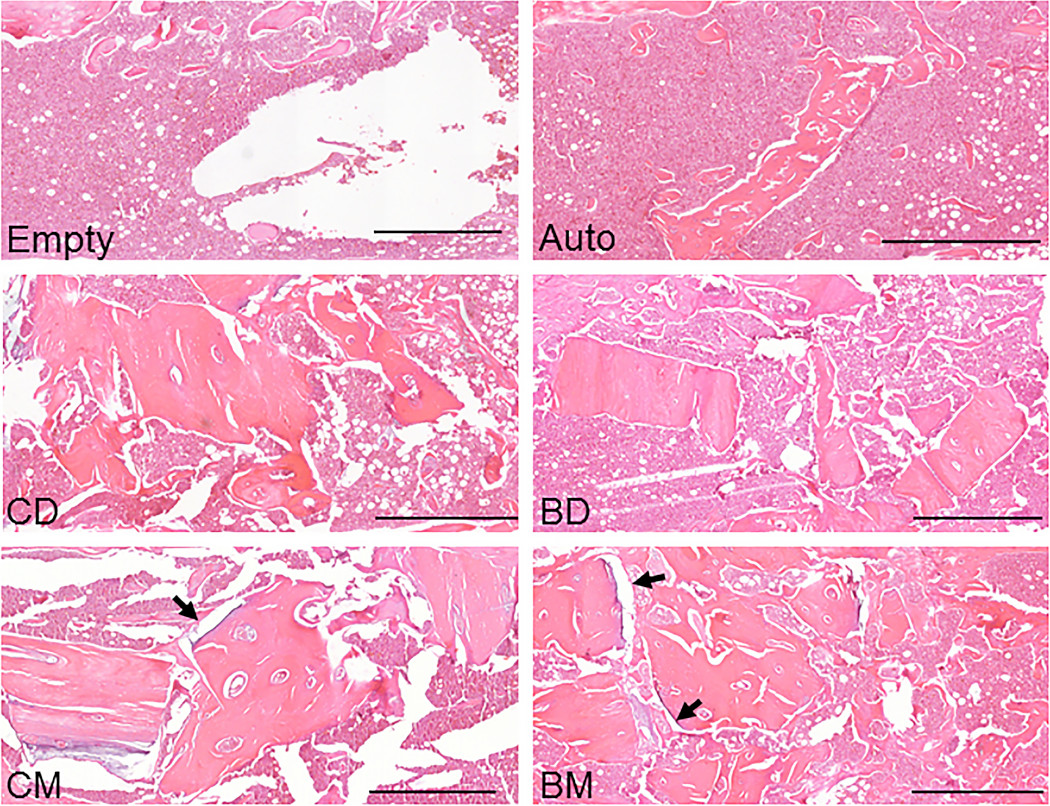
The findings of a new animal study suggest that bisphosphonate treatment in donors may indeed be relevant when mineralized allografts are used in orthopaedic procedures.
Tag: Osteoporosis

The recent JBJS Guest Editorial “What’s New in Osteoporosis and Fragility Fractures” provides an update on this important area of orthopaedic research. The authors review
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from James Blair, MD, in response to a recent edition of the OrthoJOE podcast. Geriatric
This post comes from Fred Nelson, MD, an orthopaedic surgeon in the Department of Orthopedics at Henry Ford Hospital and a clinical associate professor at
Osteoporosis is the major contributor to the increasing incidence of fragility fractures associated with low-energy falls. The other contributor is the populous baby-boomer generation that
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Shahriar Rahman, MS in response to a recent study in JAMA Internal Medicine. Hip
This post comes from Fred Nelson, MD, an orthopaedic surgeon in the Department of Orthopedics at Henry Ford Hospital and a clinical associate professor at
“We believe that bone health screening should be considered in all orthopaedic surgical candidates who are ≥50 years of age.” So proclaim Kadri et al.,
This post comes from Fred Nelson, MD, an orthopaedic surgeon in the Department of Orthopedics at Henry Ford Hospital and a clinical associate professor at
Osteoporosis is a “silent” disease, often becoming apparent only after a patient older than 50 sustains a low-energy fracture of the wrist, proximal humerus, or