The dangers of chronic opioid use have rightly been at the forefront of orthopaedic practice considerations in recent years. The widespread use of regional anesthesia and periarticular-injection cocktails, targeted NSAID utilization, and strict limitations on opioid use
Tag: spinal fusion
Postoperative fevers occur frequently. During the first 2 to 3 days after surgery, these fevers are often due to atelectasis or the increased inflammatory response
This post comes from Fred Nelson, MD, an orthopaedic surgeon in the Department of Orthopedics at Henry Ford Hospital and a clinical associate professor at
The public health crisis attributed to opioids has placed increasing emphasis on other approaches to pain management, both pharmacologic and nonpharmacologic. Although some people find
Prompted by relatively high infection rates associated with surgical treatment of pediatric spinal conditions such as scoliosis and spinal-deformity surgery in immunocompromised adults, spine surgeons
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click
OrthoBuzz regularly brings you a current commentary on a “classic” article from The Journal of Bone & Joint Surgery. These articles have been selected by the
Surgeons often prescribe more postoperative pain medication than their patients actually use. That’s partly because there is limited procedure-specific evidence-based data regarding optimal amounts and
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Brett A. Freedman, MD, in response to two recent NEJM studies on treating spondylolisthesis. The April
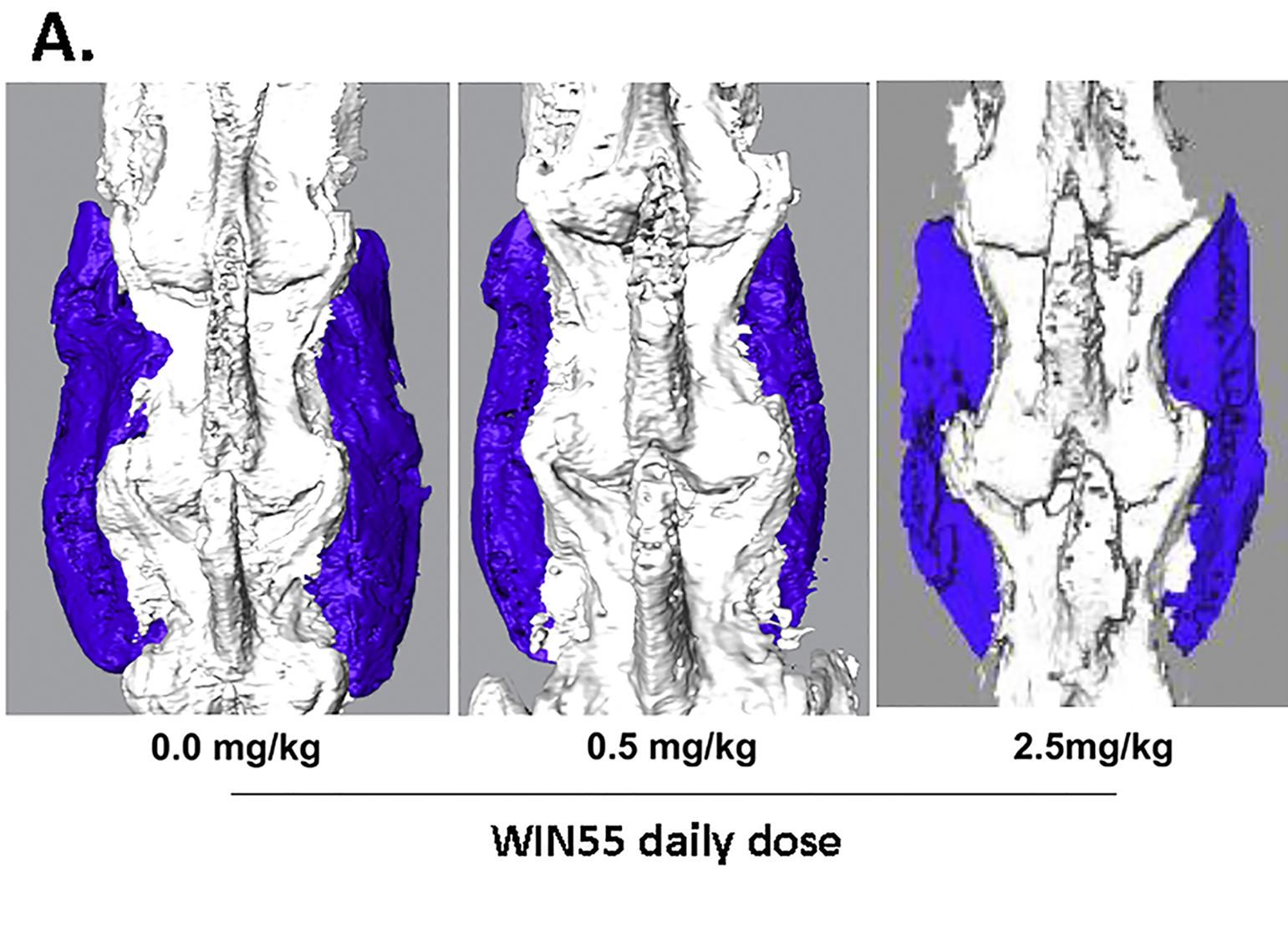
In diligent efforts to improve osseous bridges when performing spinal fusion surgery, orthopaedists have been using harvested allograft bone for more than a century and