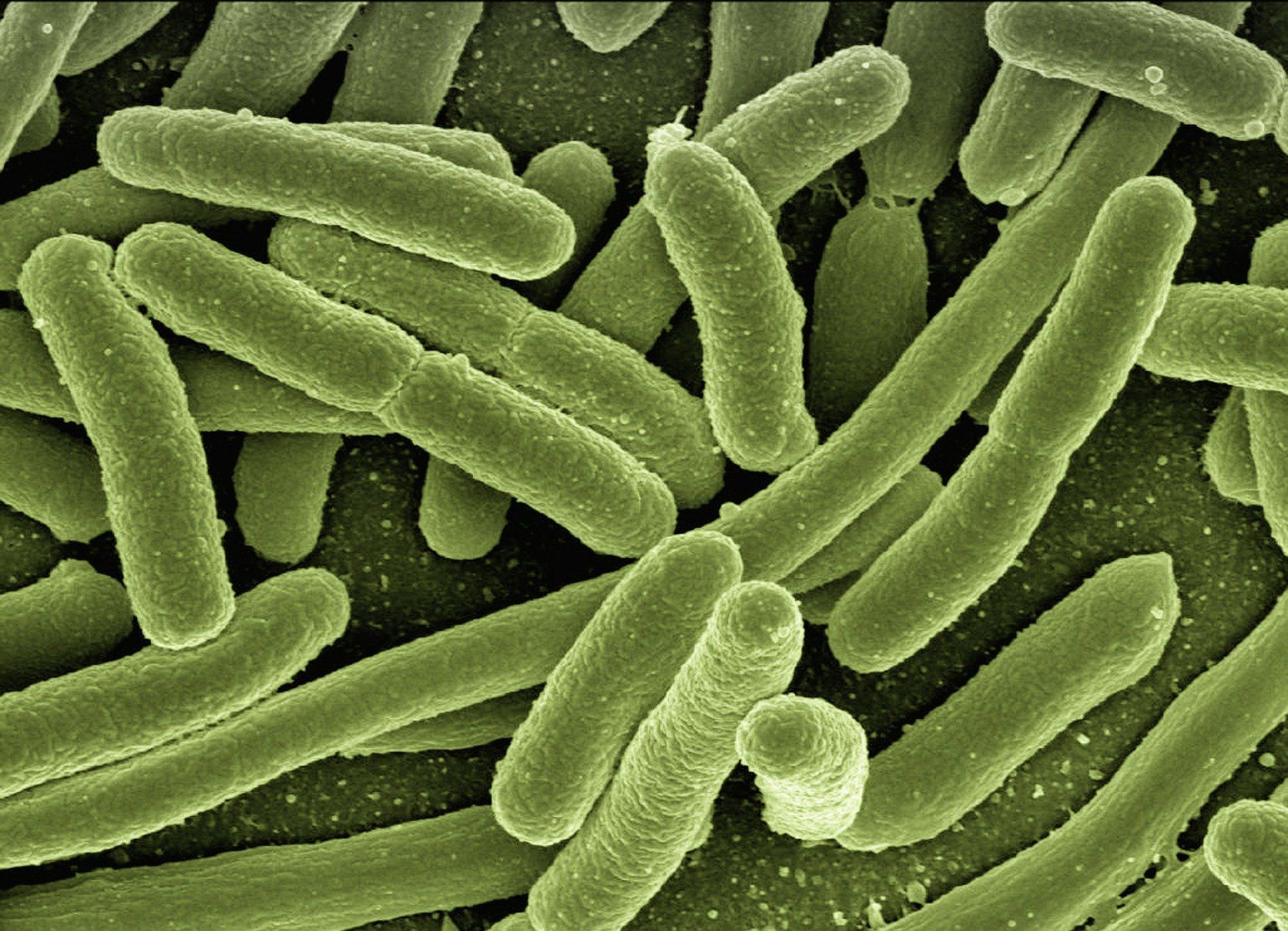
Surgical site infections (SSIs) can be devastating complications for orthopaedic patients. A new study published in Nature advances our understanding of drug-resistant pathogens that can
Tag: surgical site infection

Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 14 subspecialties. Click
Postoperative fevers occur frequently. During the first 2 to 3 days after surgery, these fevers are often due to atelectasis or the increased inflammatory response
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a
Orthopaedic educators have long confronted the subtle implication that resident participation in surgical care can contribute to patient harm or even death. While there have
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click
When >10% of patients undergoing procedures to correct a spinal deformity develop one or more surgical-site infections, investigations into how to mitigate such infections seem
In the November 18, 2015 edition of JBJS, Lawing et al. present a well-documented cohort study comparing the outcomes of open-fracture management with local administration
A recent case-control study in Foot & Ankle International found that high-risk diabetic patients (mean age of 60) undergoing reconstructive foot and/or ankle surgery were
Surgical site infections (SSIs) can cancel out the benefits of surgery, and they’re the number-one cause of hospital readmissions following surgery. The most prevalent pathogenic