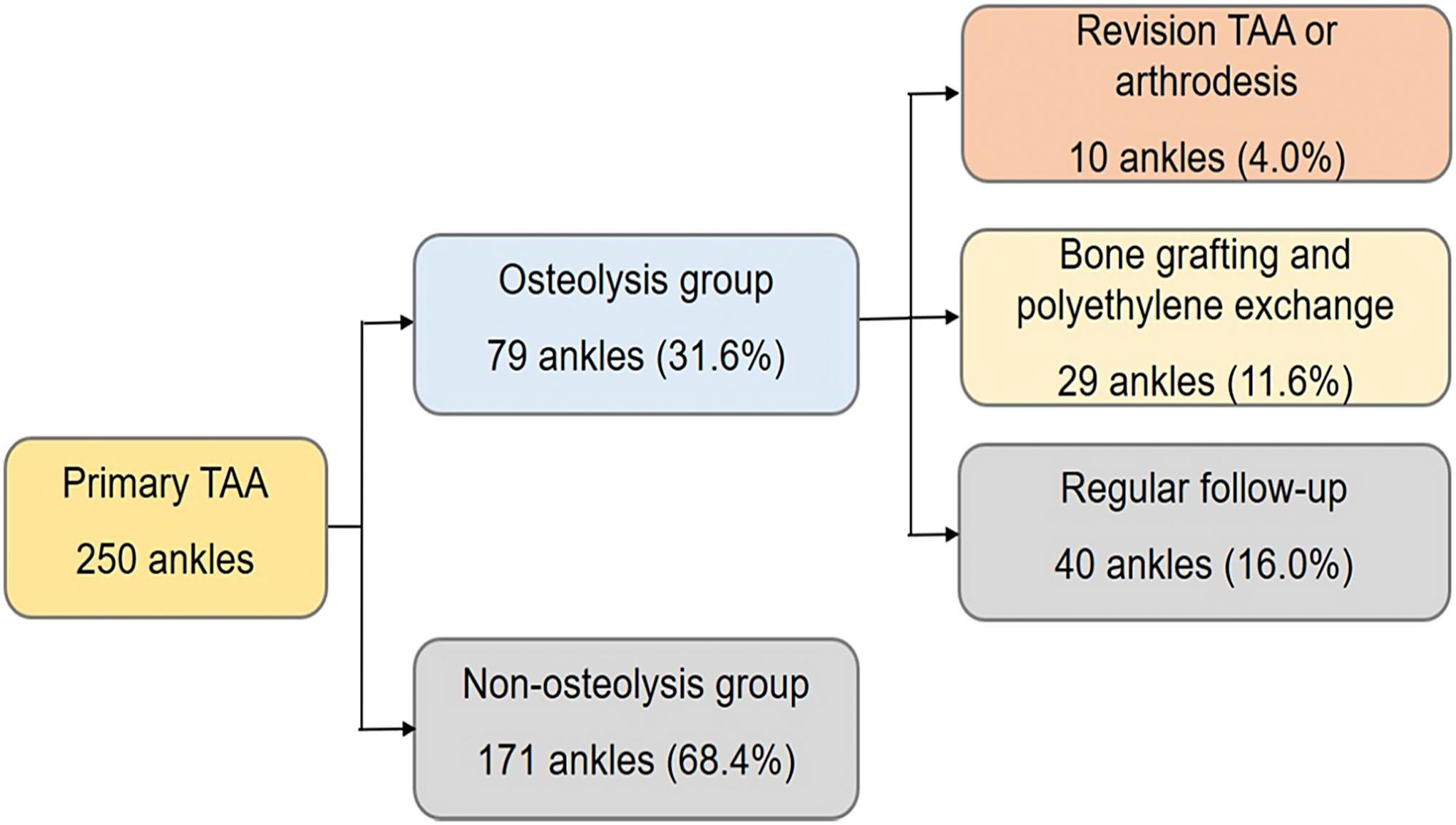
Total ankle arthroplasty (TAA) continues to gain favor as an alternative to ankle arthrodesis. However, periprosthetic osteolysis is a risk factor for a poor outcome.
Tag: TAA
As the orthopaedic community continues to solve complex issues related to joint replacement, it has become apparent that deformity correction and component positioning are keys
After some relatively poor results in the 1980s, there was a “reboot” with total ankle arthroplasty (TAA) in the late 1990s to improve outcomes so
The relationship between orthopaedic foot and ankle surgeons and podiatric surgeons has been checkered. Many have advocated that the orthopaedic community should isolate itself from
Among the many variables discussed when patients and surgeons make a decision between ankle arthrodesis (fusion) and total ankle replacement (TAA) for end-stage ankle arthritis,
We have entered an era where total ankle arthroplasty (TAA) is accepted as a rational approach for patients with degenerative arthritis of the ankle. TAA