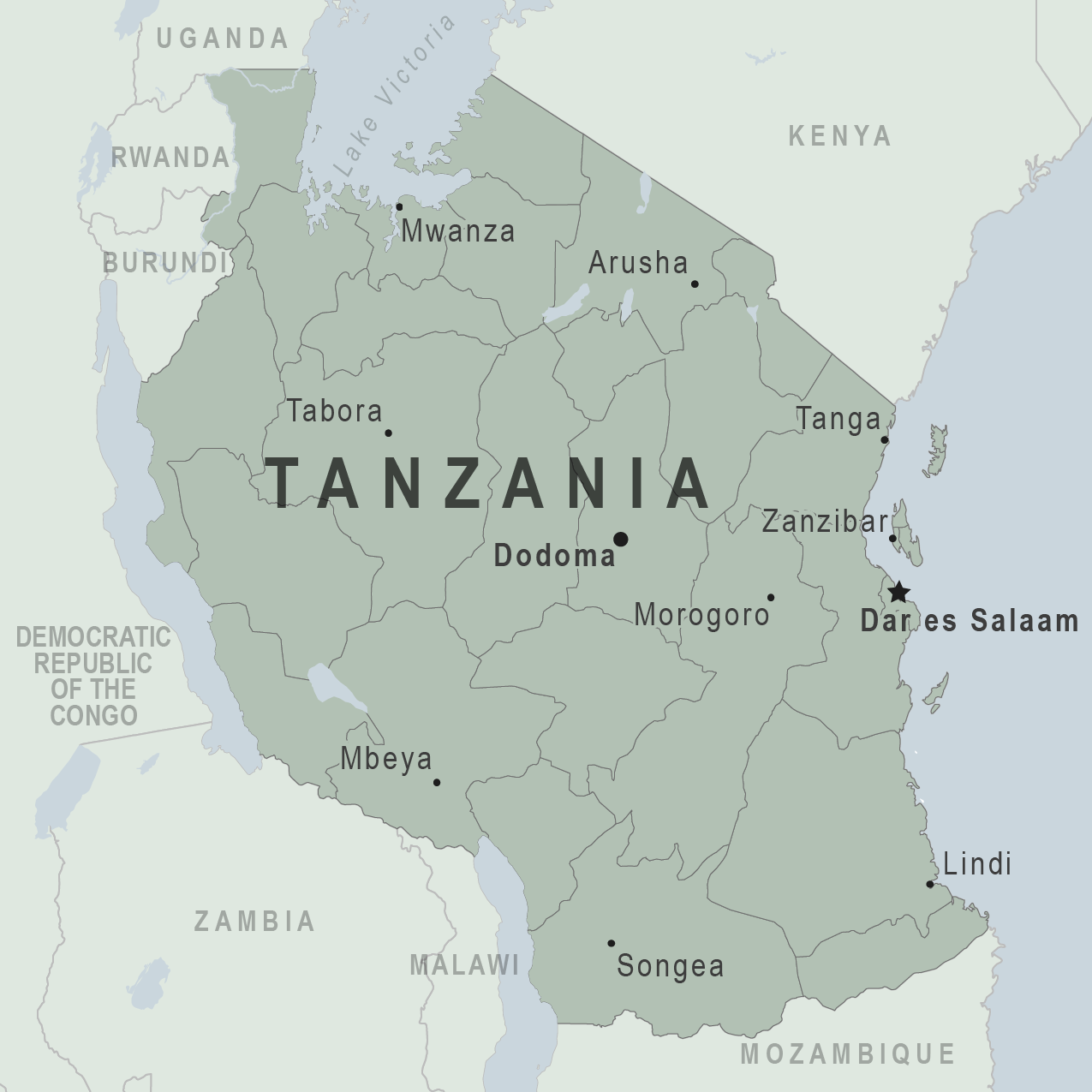
In a recent report in JBJS, Holler et al. investigated risk factors for delayed management of open tibial fractures in Tanzania. As the authors note,
Tag: tibia
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click
OrthoBuzz regularly brings you a current commentary on a “classic” article from The Journal of Bone & Joint Surgery. These articles have been selected by the Editor-in-Chief