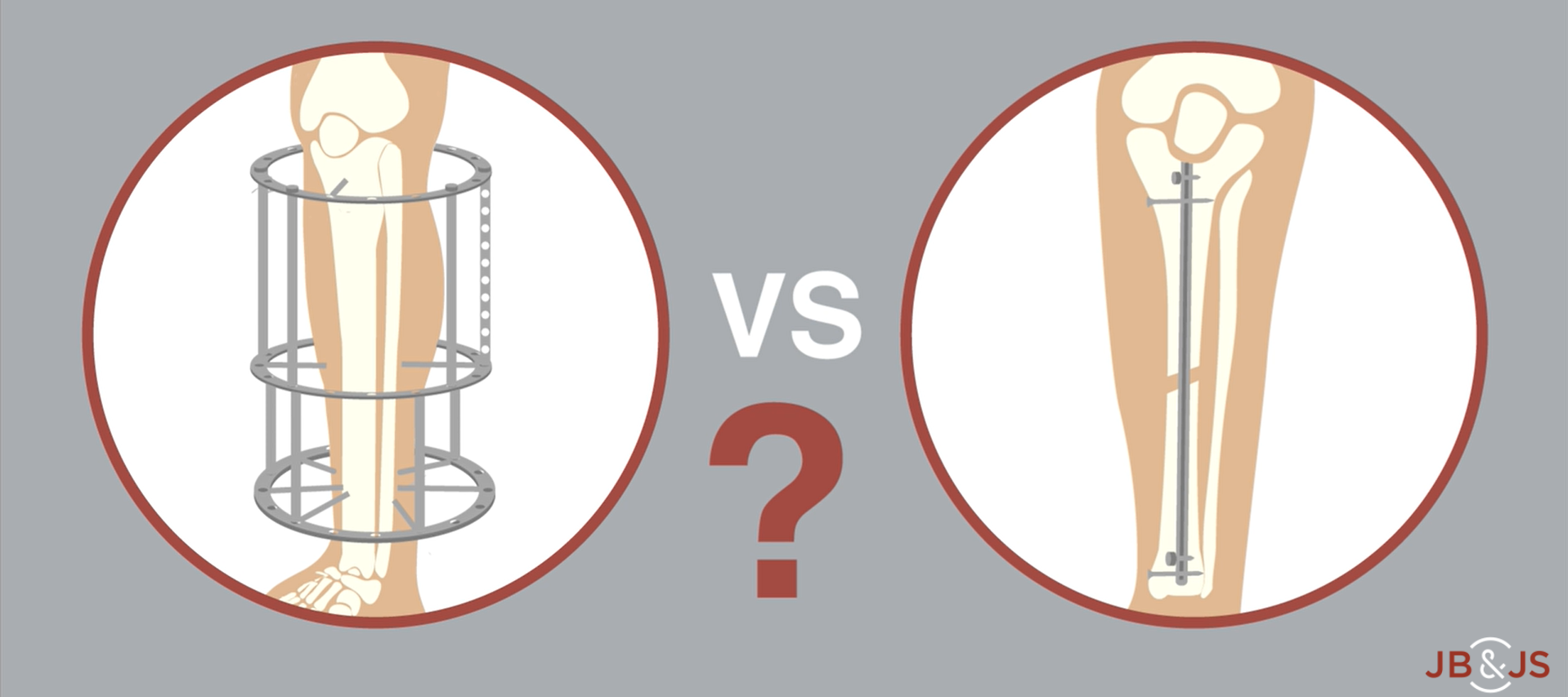
A new RCT provides Level I evidence for internal vs. external fixation of severe open tibial fractures. High-level data have been lacking until now. In
Tag: Tibial Fracture
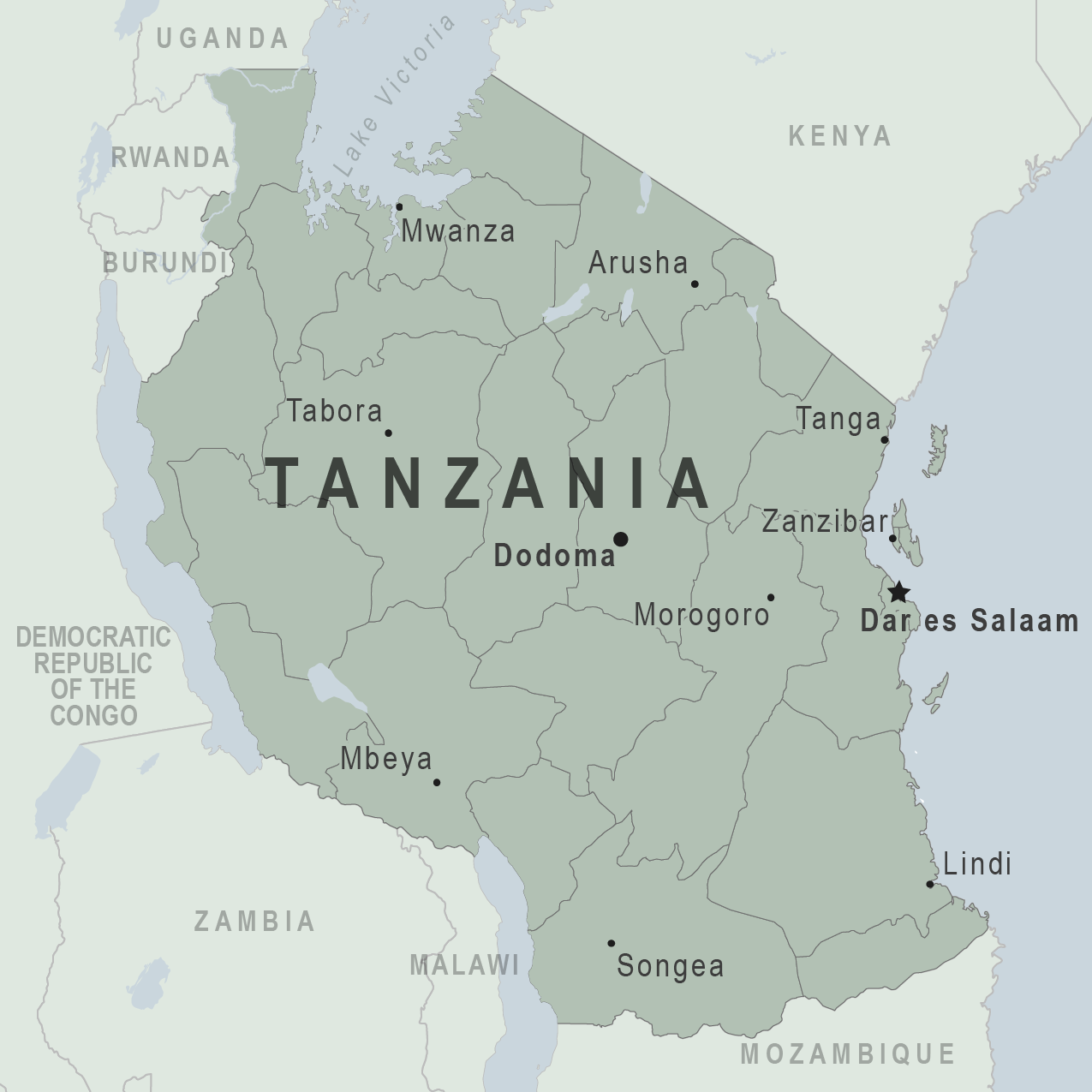
In a recent report in JBJS, Holler et al. investigated risk factors for delayed management of open tibial fractures in Tanzania. As the authors note,

JBJS Essential Surgical Techniques (EST), in collaboration with CORTICES and with the support of POSNA, is pleased to present the “JBJS EST Pediatric Trauma Collection,” an online resource of video-based articles demonstrating the surgical treatment
Many orthopaedic surgeons who take emergency-department or trauma call are confronted with a pediatric patient presenting with a fracture. However, very few of those orthopaedists are
Although many patients believe marijuana is an effective agent to treat chronic and nerve pain, the effect of cannabis on acute musculoskeletal pain has been
Generally speaking, orthopaedic surgeons in low-resourced environments deliver the best care for their patients with skill, creativity, and passion. These surgeons are accustomed to scrambling
Under one name or another, The Journal of Bone & Joint Surgery has published quality orthopaedic content spanning three centuries. In 1919, our publication was
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties.
Orthopaedic surgeons have developed a heightened awareness of the scientific evidence that supports the decisions that they make in the care of patients. Levels of