In the current issue of JBJS, Goh et al. report on the association between glucose variability and postoperative complications following aseptic revision total joint arthroplasty
Tag: TJA
Recent studies on periprosthetic joint infection (PJI) and other topics are presented in the JBJS Guest Editorial “What’s New in Musculoskeletal Infection.” Here, we spotlight
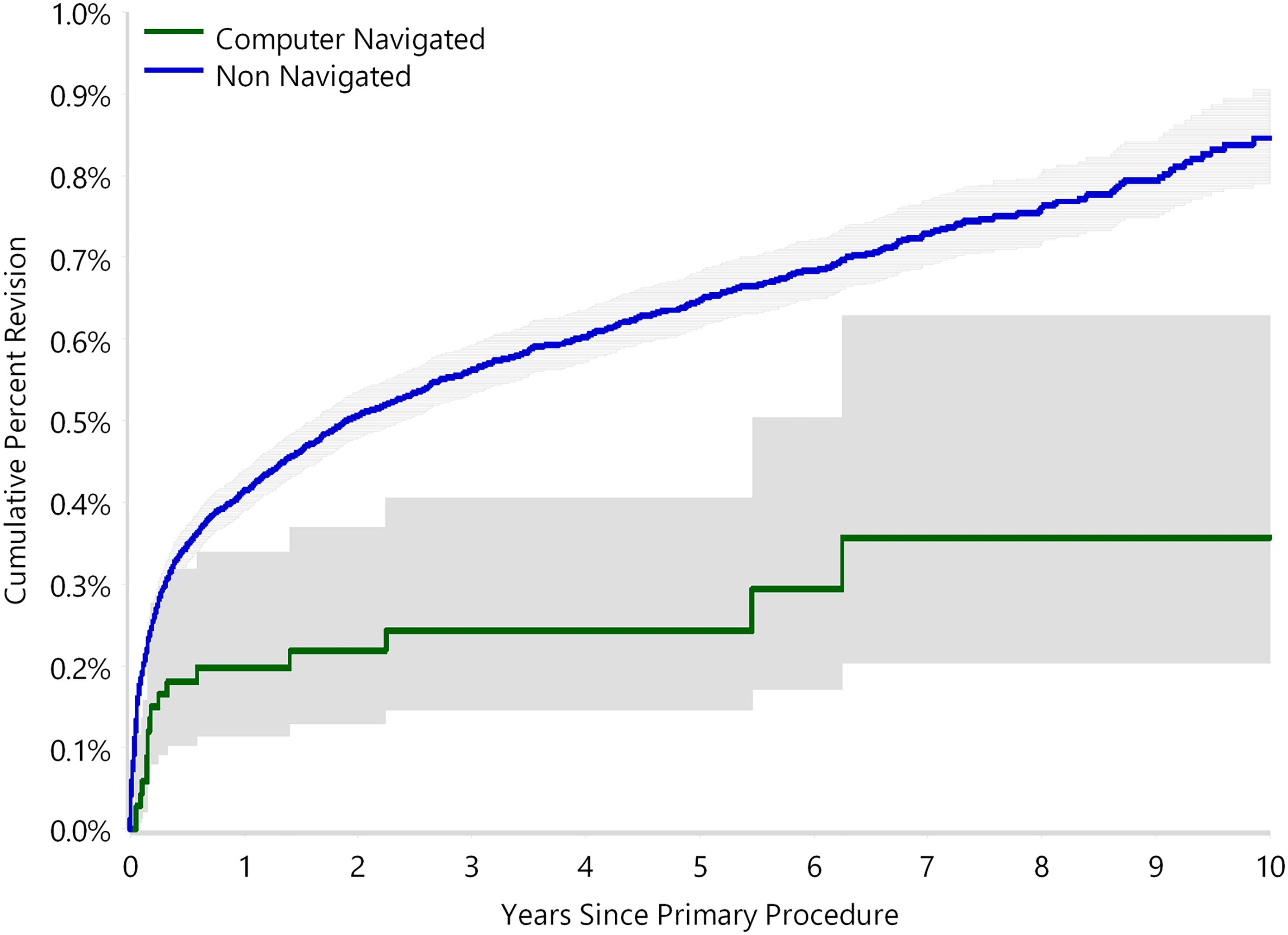
The use of computer navigation in total joint arthroplasty is increasing. Navigation has been employed less in total hip arthroplasty (THA) than in total knee arthroplasty, perhaps because of the increased need for
Over the last 2 decades, research into how various “preexisting conditions” affect the outcomes of orthopaedic interventions has increasingly focused on the impact of mental
As Fleischman et al. observe in the January 17, 2018 edition of The Journal, “there is a prevailing belief that patients living alone cannot be
Patients with diabetes have an increased risk of postoperative complications following total joint arthroplasty (TJA). Additionally, perioperative hyperglycemia has been identified as a common and
An estimated 7 million people living in the US have undergone a total joint arthroplasty (TJA), and the demand for total hip arthroplasty (THA) and
Here’s one thing about which medical studies have been nearly unanimous: Smoking is a health hazard by any measure. In the February 15, 2017 edition
A case-control study by Boraiah et al. in the December 2, 2015 JBJS describes a risk-stratification tool that helps predict which patients undergoing total joint

