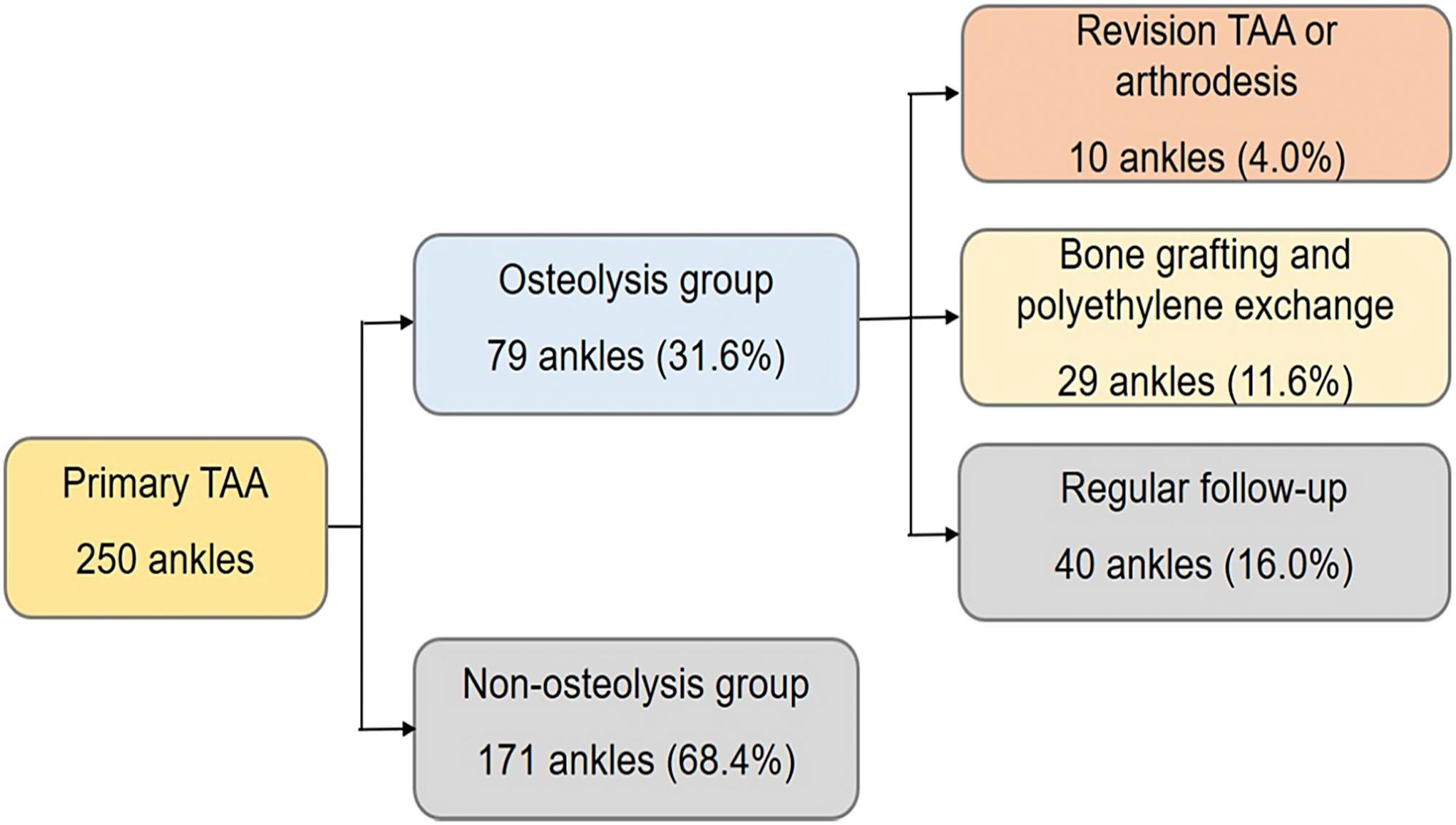
Total ankle arthroplasty (TAA) continues to gain favor as an alternative to ankle arthrodesis. However, periprosthetic osteolysis is a risk factor for a poor outcome.
Tag: total ankle arthroplasty
Ankle fusion continues to be a predictable treatment for degenerative tibiotalar arthritis. It improves both pain and function from primary osteoarthritis and degeneration related to
As the orthopaedic community continues to solve complex issues related to joint replacement, it has become apparent that deformity correction and component positioning are keys
Patients considering surgery for end-stage ankle arthritis often ask which treatment—arthroplasty or arthrodesis—will help the most. Findings from various studies attempting to answer that complex
After some relatively poor results in the 1980s, there was a “reboot” with total ankle arthroplasty (TAA) in the late 1990s to improve outcomes so
The relationship between orthopaedic foot and ankle surgeons and podiatric surgeons has been checkered. Many have advocated that the orthopaedic community should isolate itself from
It is not often that The Journal of Bone & Joint Surgery publishes an article about data-linkage efforts. To even raise the topic with most
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties.
Among the many variables discussed when patients and surgeons make a decision between ankle arthrodesis (fusion) and total ankle replacement (TAA) for end-stage ankle arthritis,
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click