Rotator cuff repair, shoulder arthroplasty, shoulder instability, and the treatment of elbow injuries are among the topics of recent studies reviewed in the new JBJS
Tag: TSA
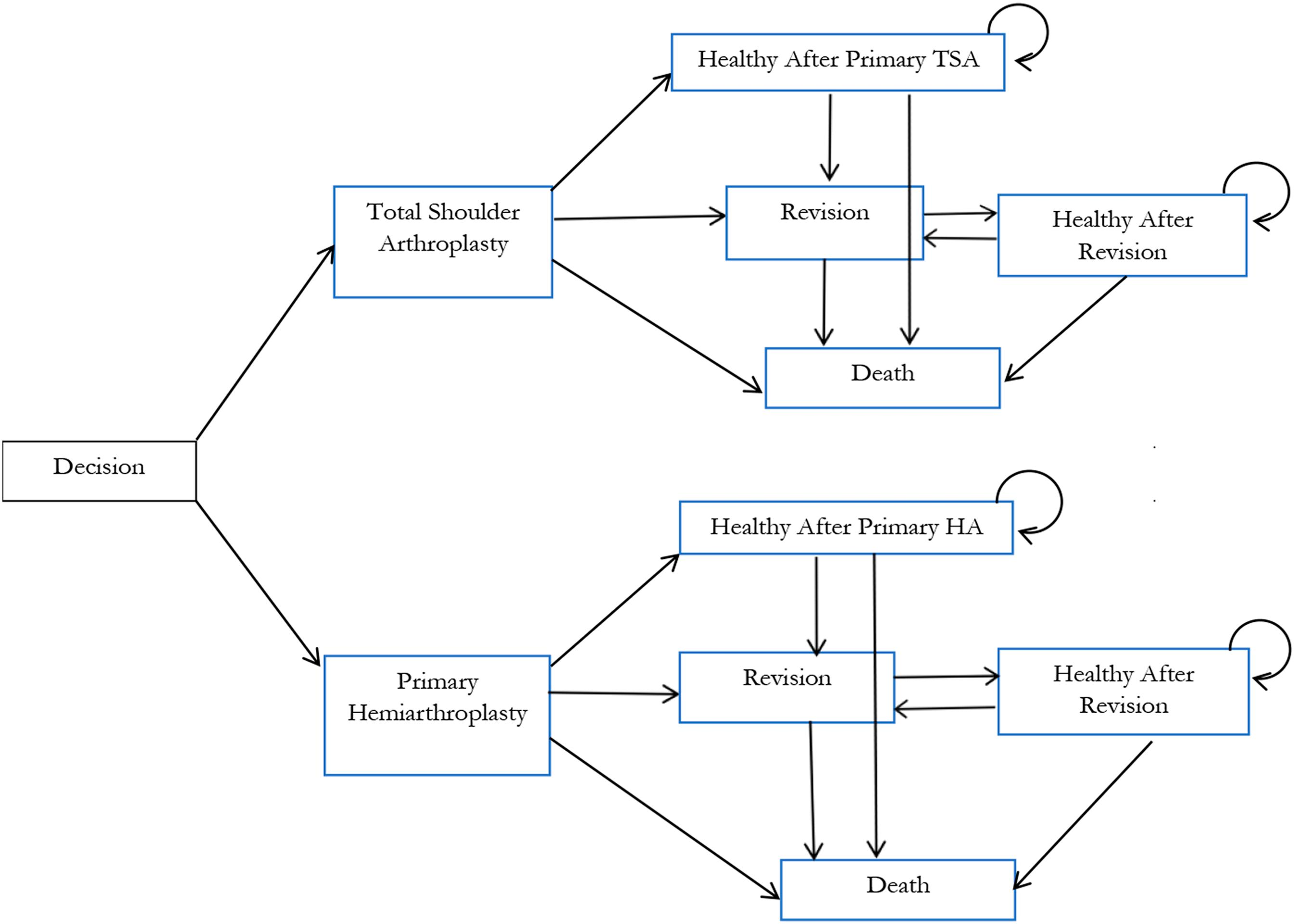
In a new study reported in JBJS, Lapner et al. conducted a cost-utility analysis of total shoulder arthroplasty (TSA) versus hemiarthroplasty from the perspective of Canada’s publicly funded health-care system. They used
The analysis did not identify evidence that the results of TSA were statistically or clinically improved over the 2 decades of study or that any
Although the indications for anatomic and reverse total shoulder arthroplasty (TSA) are different, better understanding of the rate of improvement with each type of surgery
Shoulder surgery for complex conditions such as irreparably large rotator cuff tears has been revolutionized by the concept of reverse total shoulder arthroplasty (rTSA). Improved