JBJS will have a booth at the upcoming Annual Meeting in San Diego. The conference begins today, August 31, and runs until September 4. Stop
Month: August 2021
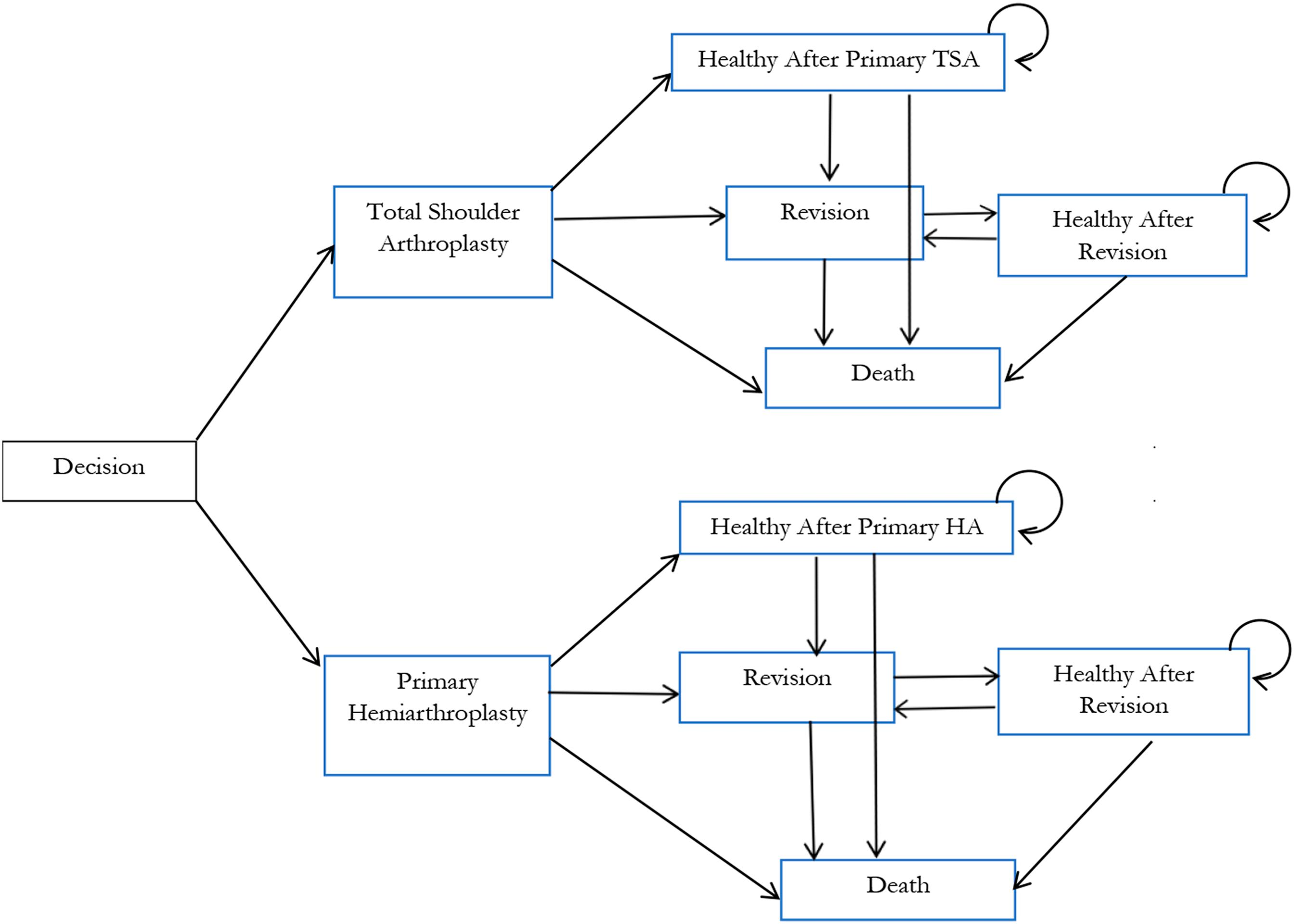
In a new study reported in JBJS, Lapner et al. conducted a cost-utility analysis of total shoulder arthroplasty (TSA) versus hemiarthroplasty from the perspective of Canada’s publicly funded health-care system. They used
Co-author Jeremy Smith, MD discusses the new JBJS study “Correlation Between Patient-Reported Outcome Measures and Health Insurance Provider Types in Patients with Hip Osteoarthritis.” Watch

Every month, JBJS publishes a review of the most pertinent and impactful studies reported in the orthopaedic literature during the previous year in 14 subspecialty areas. Click here for a collection of all such OrthoBuzz Guest
Anterior cruciate ligament (ACL) injuries once were career-ending for athletes. With the advent of ACL reconstruction, elite athletes have been able to continue to compete at the
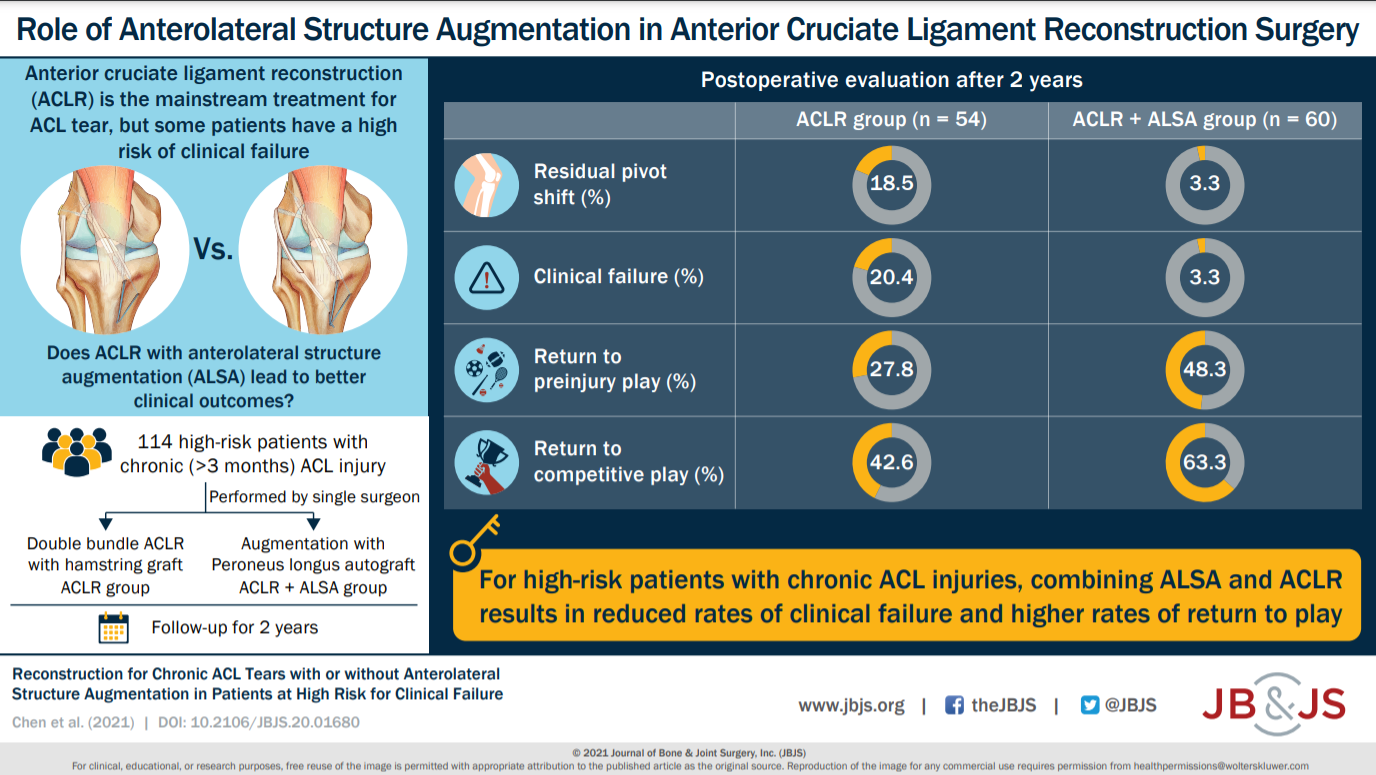
Compared with isolated ACLR, combined ACLR and ALSA resulted in a reduction in persistent rotatory laxity and higher rates of return to preinjury and competitive
Approximately 18% of JBJS scientific studies published in 2020 were Level I or II investigations. The number of high-level studies has continued to grow slowly year over year.
Our study demonstrated no short-term impact of NSAIDs/COX-2 inhibitors on long-bone fracture-healing. However, continued use of these medications for a period of >3 weeks may

JBJS Open Access (JBJS OA) is an international, peer-reviewed, open-access journal from the publishers of The Journal of Bone & Joint Surgery. The mission of this continuously published
JBJS Essential Surgical Techniques (EST) and The Journal of Bone and Joint Surgery (JBJS) give out two annual awards–one for the best Subspecialty Procedure (SP) video article, and the other
