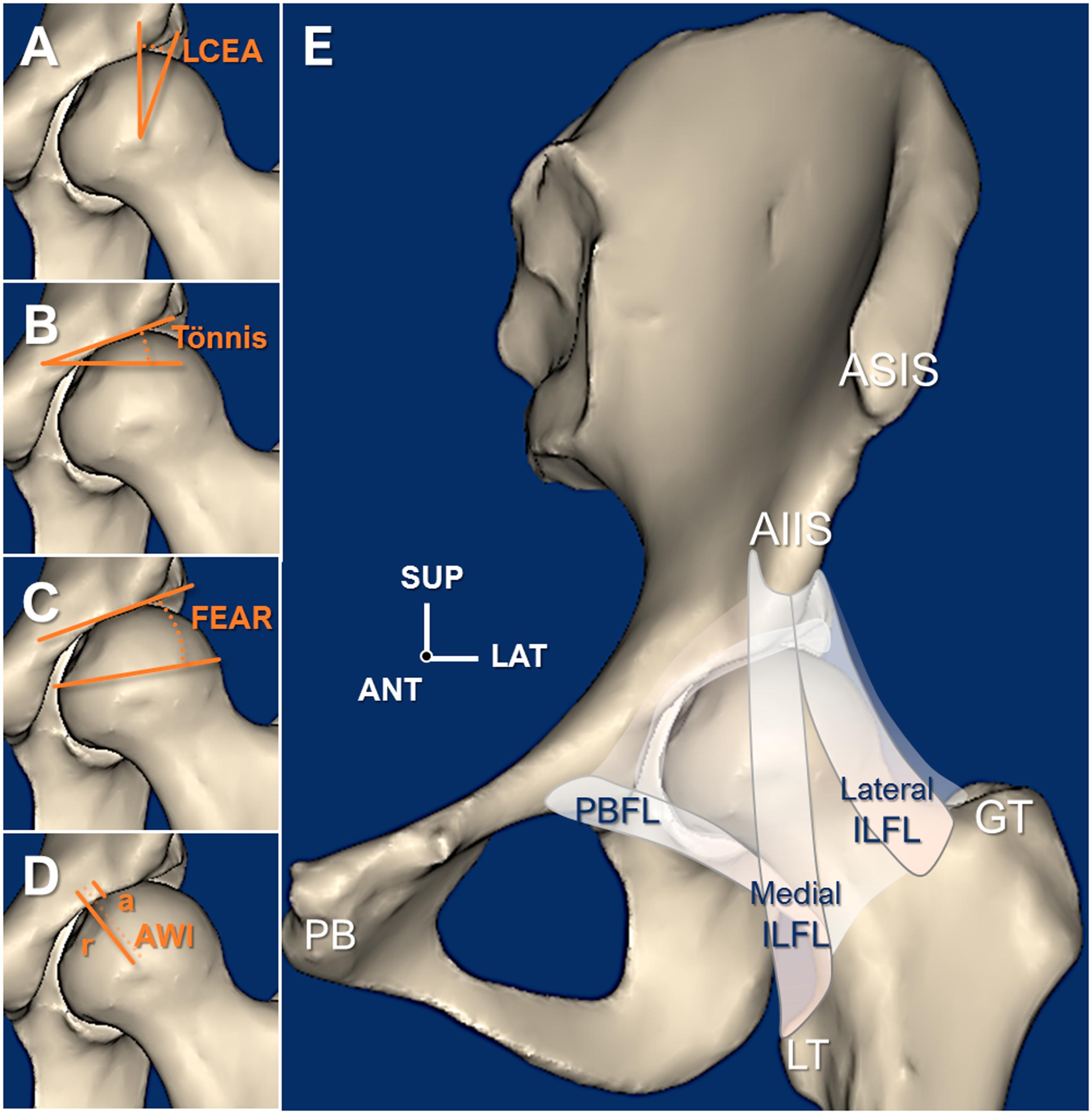
Hip dysplasia is known to cause early joint deterioration, instability, and pain. It can be corrected with the Bernese periacetabular osteotomy (PAO). However, stability of the hip isn’t only due to osseous coverage. The soft tissues, such as the capsule, also play a role.
In the current issue of JBJS, a study by Ng et al. sheds light on capsular mechanics and range of motion after PAO. The investigators hypothesized that capsular restraints may be altered after PAO and lead to changes in range of motion.
This was a cadaveric study of 12 hips with dysplasia. Nine of the hips came from female donors and 3 from male donors. The average donor age was 34 years.
The specimens were dissected down to bone and capsule and then mounted on a robotic tester. Using 5 Nm of torque, the hips underwent internal rotation (IR), external rotation (ER), abduction, and adduction in the following positions:
- Maximal extension
- Neutral 0°
- Flexion of 30°
- Flexion of 60°
- Flexion of 90°
PAO was then performed to correct the dysplasia. The capsular ligaments were preserved. Each specimen was retested in the same positions.
Following PAO, the authors found that there were changes in the motion profiles of the specimens:
Internal and External Rotation
- IR in 90° of flexion decreased by 5° (p = 0.003).
- ER in 60° of flexion increased by 7° (p = 0.001).
- ER in 90° of flexion increased by 11° (p = 0.001).
Abduction and Adduction
- Abduction in extension decreased by 10° (p = 0.002).
- Abduction in neutral decreased by 7° (p = 0.001).
- Abduction in 30° of flexion decreased by 8° (p = 0.001).
- Adduction in neutral increased by 9° (p = 0.001).
- Adduction in 30° of flexion increased by 11° (p = 0.002).
- Adduction in 60° of flexion increased by 11° (p = 0.003).
The authors highlight that the increases in hip adduction in neutral to mid-flexion and in external rotation in deep flexion were larger than the corresponding decreases in abduction and internal rotation. This indicates that the capsule also plays a role in hip stability. Even with proper correction of the osseous acetabulum, there can be increased range of motion (ER in flexion and adduction in neutral to mid-flexion) that can play a role in symptomatic hip instability.
The authors note that the capsule “may be unable to provide the needed restraint in certain femoral positions after PAO.”
Clearly, we shouldn’t change our practice from a single cadaveric study. But the authors’ findings do show that both the static and dynamic stabilizers of the hip are important. Perhaps we can’t achieve optimal outcomes by only trying to correct or normalize one (while ignoring the other). Surgery addressing osseous concerns may still require optimization of the capsular structures. And likewise for procedures treating the capsule, we must be mindful of the osseous contributions to hip stability as well.
Access the full report by Ng et al.
JBJS Deputy Editor for Social Media