In this post, Dr. Matt Schmitz, JBJS Deputy Editor for Social Media, discusses a new study examining the impact of social determinants of health on diagnostic delay in slipped capital femoral epiphysis (SCFE).
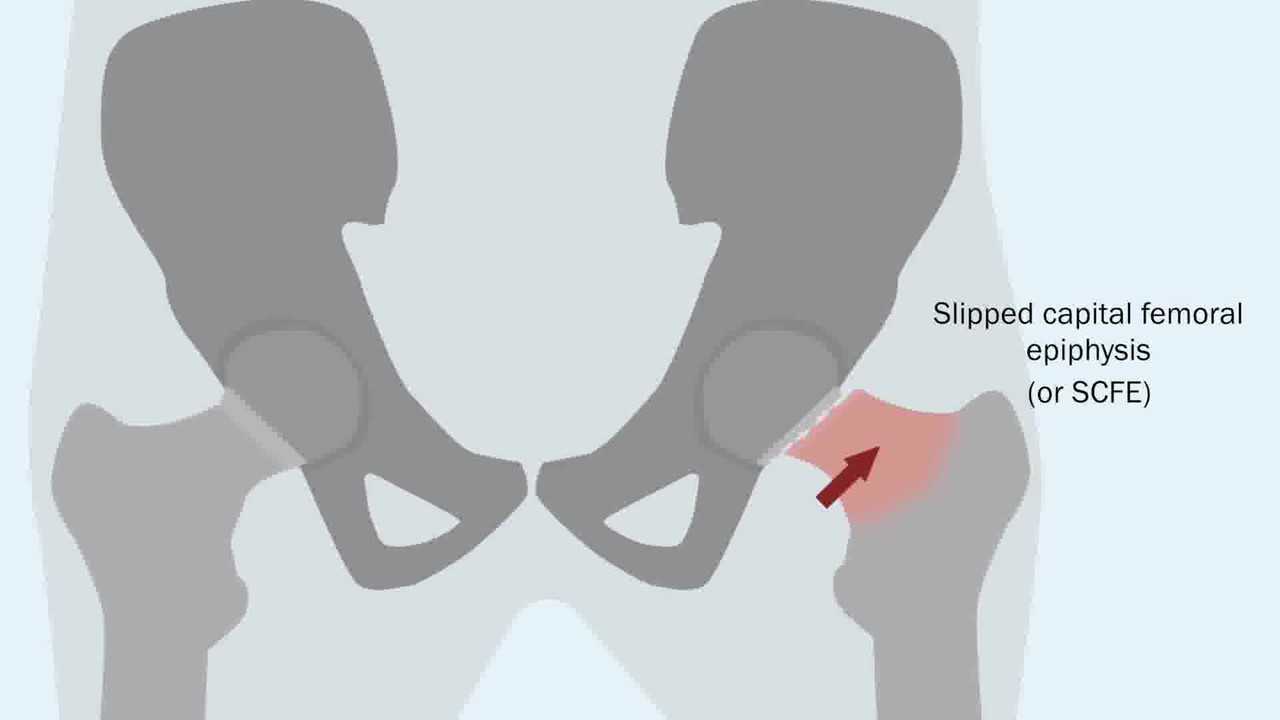
Slipped capital femoral epiphysis (SCFE) is an adolescent hip condition that can potentially lead to long-term deterioration of the hip joint. Unstable slips are usually diagnosed relatively quickly because of the child’s inability to ambulate, but with stable slips, diagnosis may be delayed because of vague symptoms and referred pain to the knee. Delays in diagnosis can lead to worsening displacement, contributing to deformity of the natural sphericity of the femoral head-neck junction and osteoarthritis.
Little is known about the predictors of delays in diagnosis, but social determinants of health are thought to potentially play a role in delay. Lack of access to medical care, insurance coverages, and even family structure have been shown to lead to disparities in health care, with further elucidation needed regarding the impact of these factors on diagnostic delay in SCFE.
In the November 1, 2023 issue of JBJS, Smith et al. present the results of a study performed at Boston Children’s Hospital in which they examined the relationships between delay in SCFE diagnosis and insurance type (public or private), family structure (single-guardian or multiguardian household), and neighborhood-level socioeconomic vulnerability (Social Vulnerability Index, or SVI, calculated at the Census-tract level). The study is now available at JBJS.org:
In this retrospective cohort study, the authors defined a delay in diagnosis as ≥12 weeks from symptom onset. They dichotomized delay based on the proportion of patients with a severe slip; only 2% of patients with a delay of <12 weeks had a severe slip, while that rate jumped to 30% with a delay of ≥12 weeks, suggesting 12 weeks as a clinically meaningful threshold. The SVI, which has been validated by the Centers for Disease Control and Prevention, was dichotomized ( ≥0.75 vs. <0.75) to compare patients in the highest quartile vs. those in the lowest 3 quartiles of vulnerability.
Study Highlights
Overall, 351 patients underwent surgical fixation for a stable SCFE from 2002 to 2021. The mean patient age at presentation was 12 years, 60% of the patients were male, 61% were White, and 64% were obese.
Thirty-seven percent (129) of the patients had a diagnostic delay of ≥12 weeks. Delay was associated with increased slip severity, obesity, younger age at symptom presentation, physician specialty of orthopaedic surgeon at the time of presentation, and ≥3 interactions with the health-care symptom prior to diagnosis.
In multivariable analyses:
- Patients with public insurance were more likely to have a diagnostic delay compared with patients with private insurance (OR, 1.83 [95% CI, 1.12 to 2.97]; p = 0.015).
- Patients in single-guardian households were more likely to have a delay compared with patients in multiguardian households (adjusted OR, 1.95 [95% CI, 1.11 to 3.45]; p = 0.021).
- The researchers did not find a significant increase in the odds of delay for patients in the highest quartile of overall SVI compared with those in the lower 3 quartiles.
Diagnostic Delays Persist
It has been documented in multiple studies that a lack of private insurance can lead to delays in orthopaedic care. This paper adds new data regarding the association of public insurance and delay in SCFE diagnosis. The authors note that additional research is needed “to understand if SCFE-specific care is denied or delayed for those with less generous insurance or if insurance is a proxy for other factors or behaviors that lead to delay.”
To the researchers’ knowledge, this is the first investigation to assess the role of family structure in SCFE diagnosis. There are a number of potential reasons for the association found for single-guardian status, including difficulties in scheduling and attending orthopaedic referral appointments due to work schedule, lower economic resources, or fewer parent-child interactions, but the study also highlights the importance of orthopaedic education in primary care. The authors note that 72.5% of patients diagnosed by orthopaedic surgeons had at least 2 prior interactions with the health-care system. Delay in diagnosis is compounded when you take into account the difficulty of obtaining and scheduling an orthopaedic appointment if a diagnosis is still unknown.
Clearly there are social factors that influence delays in orthopaedic care. Dr. Kanu Okike offers further reflection on interpreting the results of this study in a related commentary article: Social Determinants of Delay.
As orthopaedic surgeons, we must focus on helping our most vulnerable patients. Knowing that hip conditions like SCFE can lead to long-term disability issues, it is imperative that we increase our understanding of social determinants of health that contribute to diagnostic delay and address disparities in care in order to best serve our patients.
Read the study by Smith et al. at JBJS.org:
JBJS Deputy Editor for Social Media