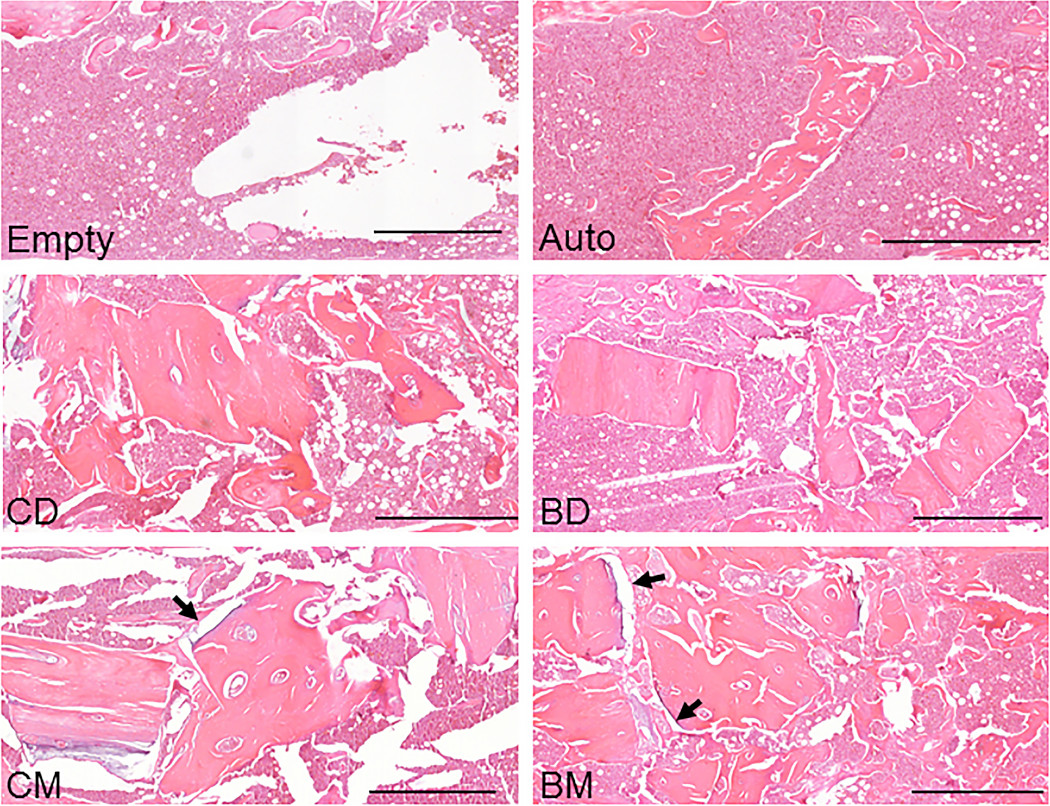
The findings of a new animal study suggest that bisphosphonate treatment in donors may indeed be relevant when mineralized allografts are used in orthopaedic procedures.
Tag: allograft
For the last 6 years, JBJS has participated in an “article exchange” collaboration with the Journal of Orthopaedic & Sports Physical Therapy (JOSPT) to support multidisciplinary integration, continuity of
Allograft bone is used often in orthopaedic surgery. However, the use of structural allografts to address large acetabular defects in total hip arthroplasty (THA) is
Under one name or another, The Journal of Bone & Joint Surgery has published quality orthopaedic content spanning three centuries. In 1919, our publication was
In a population-based epidemiological study published in the July 6, 2016 Journal of Bone & Joint Surgery, Tibor et al. found that from 2007 to
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties.
For decades, researchers have been investigating different methods of cartilage repair, but no approach has yet risen to “gold standard” status. In the June 24,
Attempts by orthopaedists to repair torn human ACLs have failed for the most part, so surgeons now rely almost exclusively on removing the torn ligament