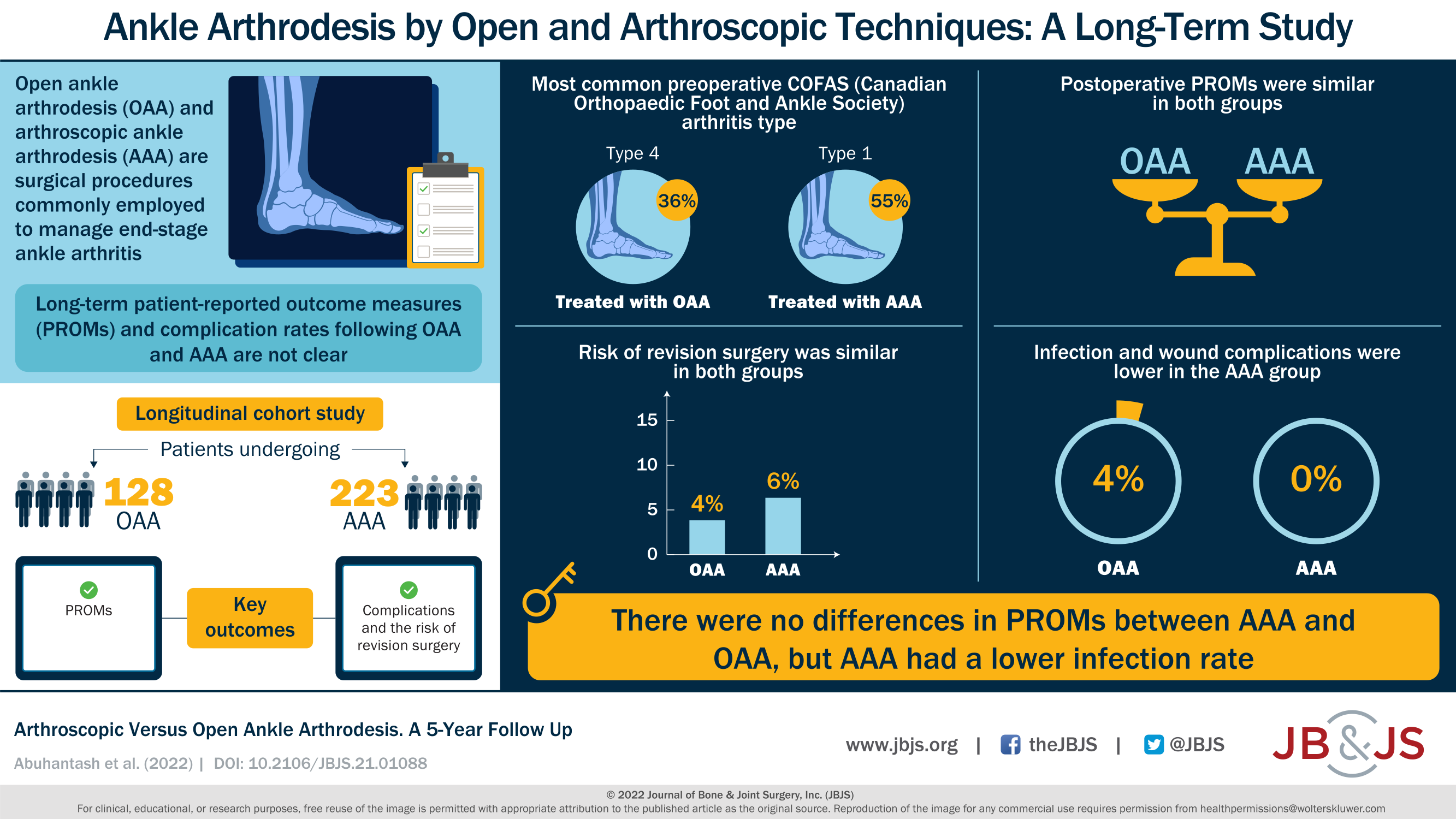
A new JBJS report compares arthroscopic versus open ankle arthrodesis. The authors analyzed long-term patient-reported outcomes, major complications, and reoperations. JBJS Editor-in-Chief Dr. Marc Swiontkowski
Tag: arthrodesis
Ankle fusion continues to be a predictable treatment for degenerative tibiotalar arthritis. It improves both pain and function from primary osteoarthritis and degeneration related to
Patients considering surgery for end-stage ankle arthritis often ask which treatment—arthroplasty or arthrodesis—will help the most. Findings from various studies attempting to answer that complex
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Shahriar Rahman, MS, in response to a recent study in Foot and Ankle Clinics of North
Under one name or another, The Journal of Bone & Joint Surgery has published quality orthopaedic content spanning three centuries. In 1919, our publication was
Among the many variables discussed when patients and surgeons make a decision between ankle arthrodesis (fusion) and total ankle replacement (TAA) for end-stage ankle arthritis,
We have entered an era where total ankle arthroplasty (TAA) is accepted as a rational approach for patients with degenerative arthritis of the ankle. TAA
In the December 7, 2016 issue of JBJS, Krause et al. analyze data from a 2013 industry-sponsored RCT to investigate correlations between nonunions of hindfoot/ankle
Most studies looking into revision rates after cervical spine fusion follow patients for 2 to 5 years. But in the September 21, 2016 issue of
A therapeutic Level II study by DiGiovanni et al. in the August 3, 2016 edition of The Journal of Bone & Joint Surgery examined the