Implant design, socioeconomic inequality, and opioid prescriptions are some of the topics of the recent studies summarized in the JBJS Guest Editorial “What’s New in
Tag: hemiarthroplasty

This commentary comes from guest contributor Matthew Deren, MD, in response to a recent study in The New England Journal of Medicine. To cement or
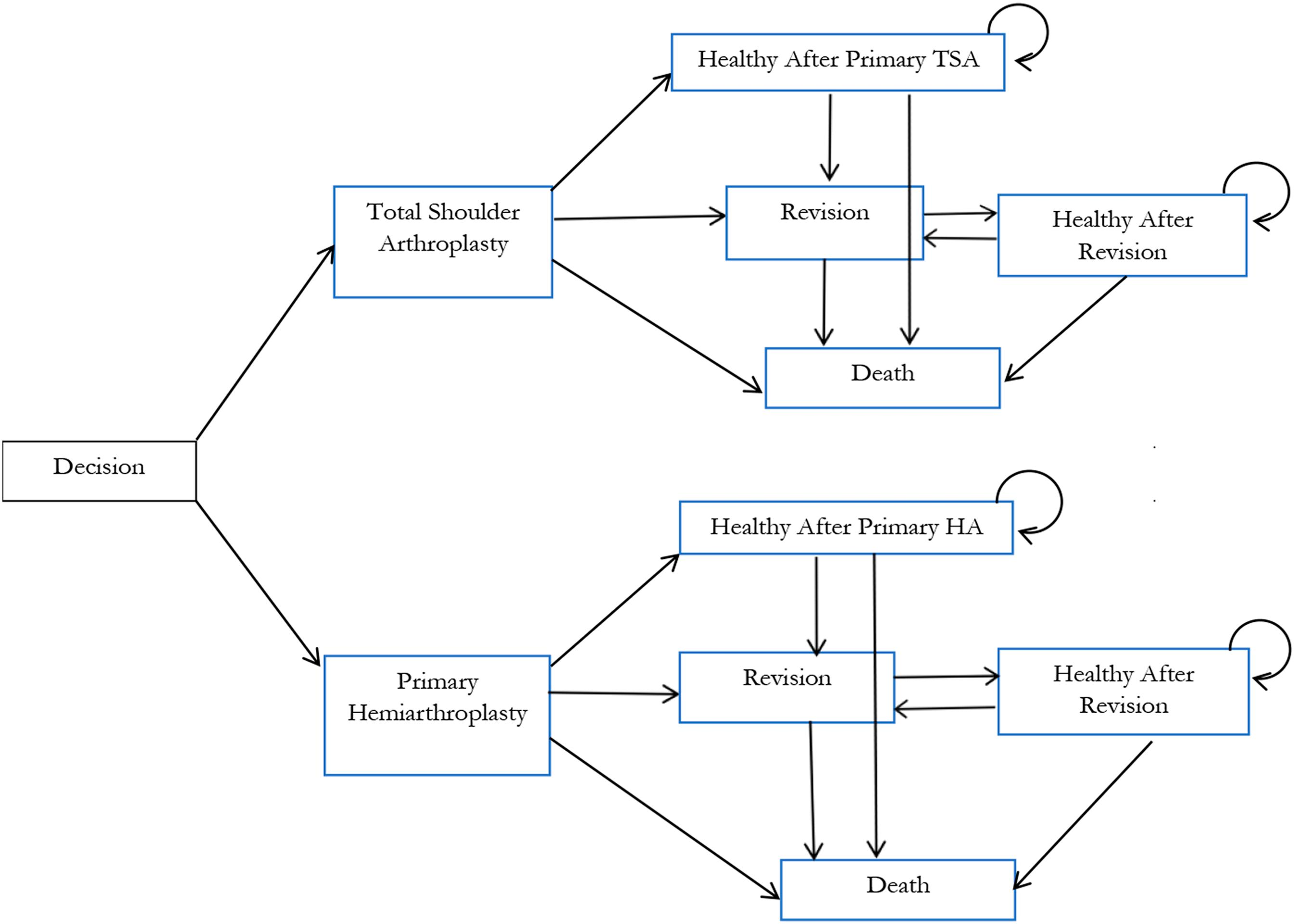
In a new study reported in JBJS, Lapner et al. conducted a cost-utility analysis of total shoulder arthroplasty (TSA) versus hemiarthroplasty from the perspective of Canada’s publicly funded health-care system. They used

Every month, JBJS publishes a review of the most pertinent and impactful studies reported in the orthopaedic literature during the previous year in 14 subspecialties. Click here for a collection of all such OrthoBuzz specialty-update summaries. This
Consulting with their patients, orthopaedic surgeons make many decisions each day by weighing the best evidence available. One frequent—and controversial—decision is how best to treat displaced femoral
Predicting life expectancy is not an exact science. But estimating the remaining years of life in elderly patients with a femoral neck fracture may help
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for
OrthoBuzz occasionally receives posts from guest bloggers. In response to a recent study in The New England Journal of Medicine, the following commentary comes from Paul E. Matuszewski,
Trying to educate elderly patients and their family members about how to best treat a femoral neck fracture can be difficult. These patients typically have
In the January 4, 2017 issue of The Journal, Swart et al. provide a well-done Markov decision analysis on the cost effectiveness of three treatment

