JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers
Tag: JBJS
JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers

JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers
JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers
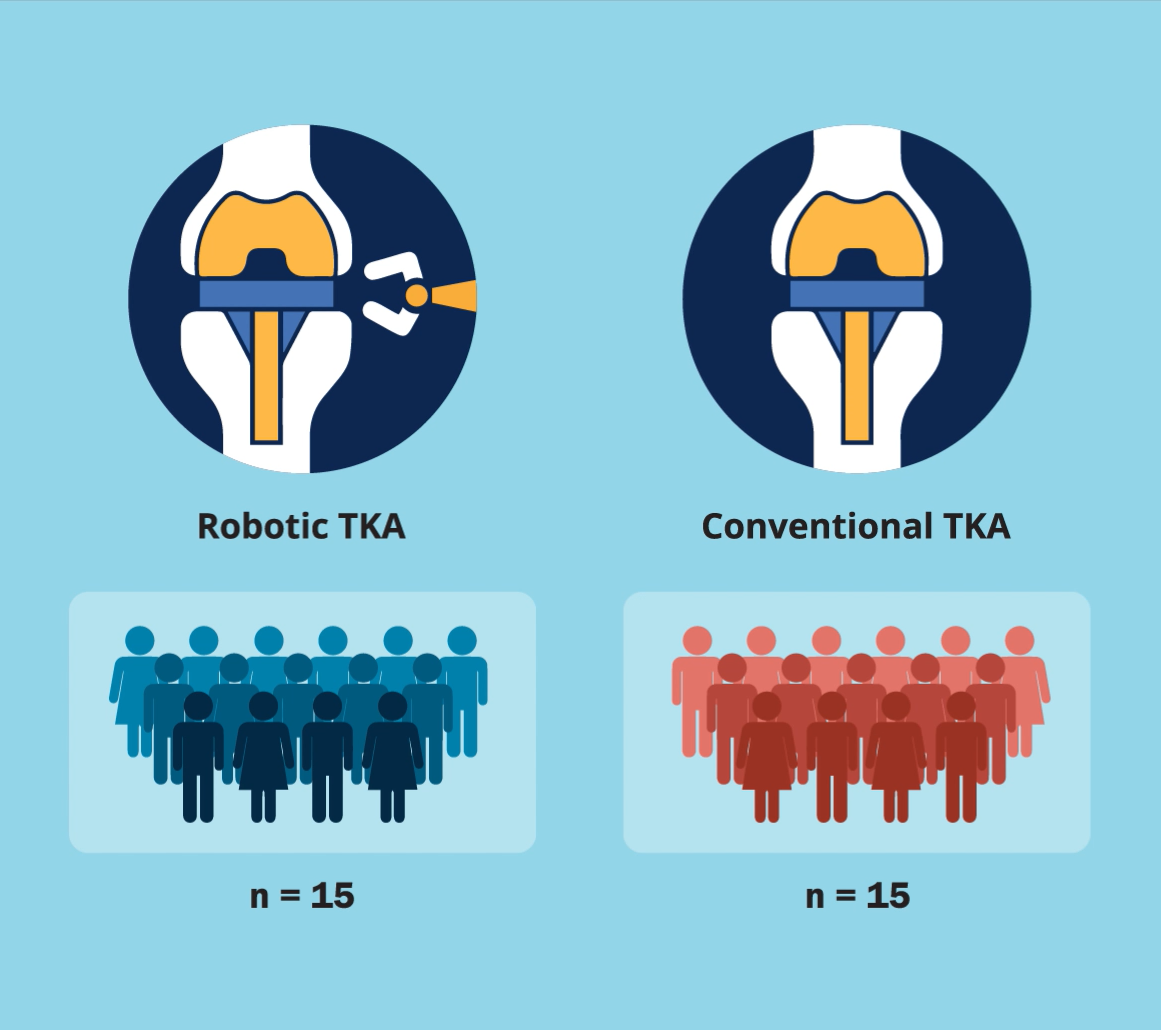
A new JBJS study by Fontalis et al. compares the inflammatory response in robotic-arm-assisted total knee arthroplasty (TKA) vs. conventional jig-based TKA. The investigators also
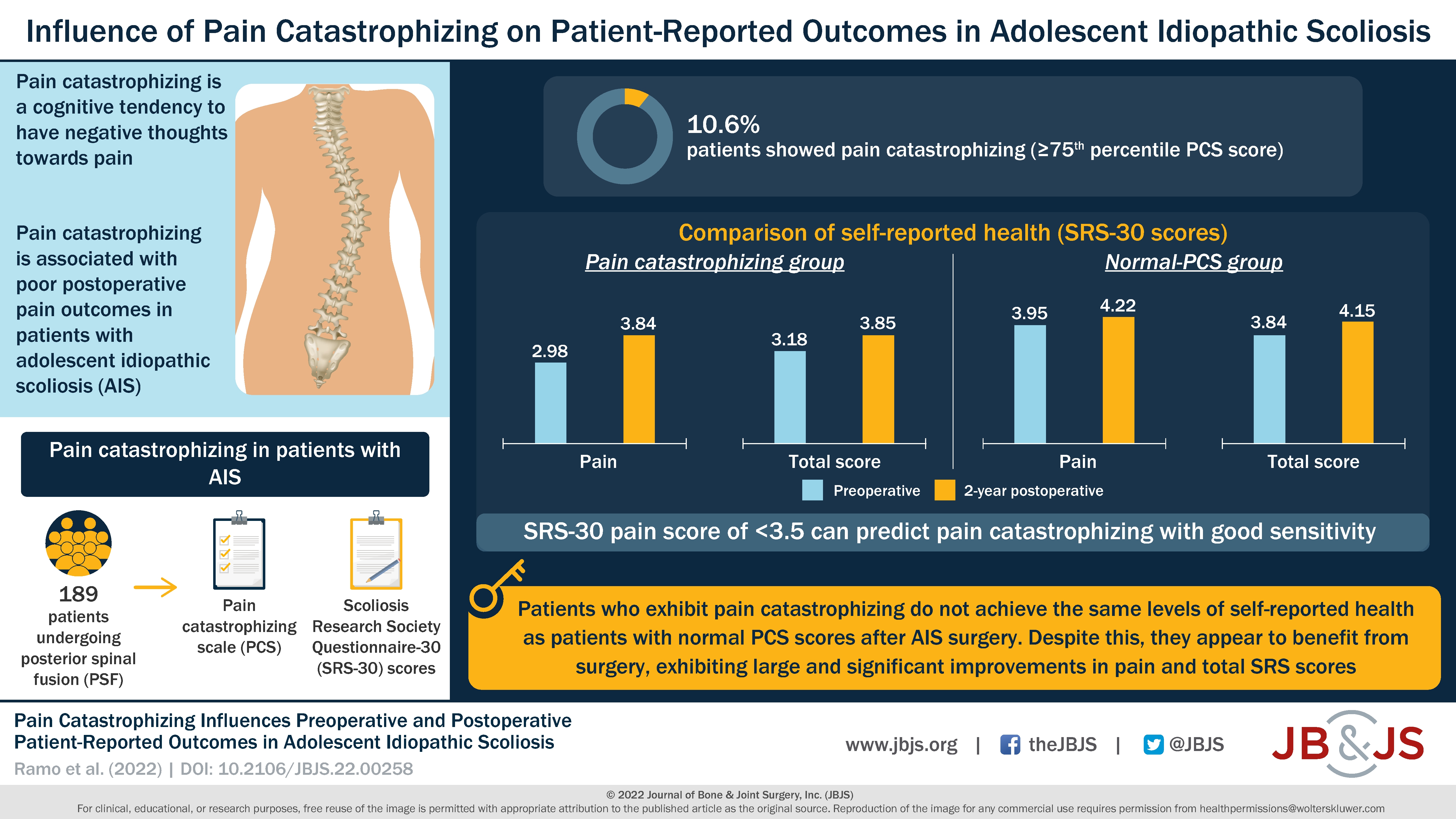
In this OrthoBuzz post, Editor-in-Chief Dr. Marc Swiontkowski reflects on a new JBJS study that examines pain catastrophizing among patients with adolescent idiopathic scoliosis (AIS).
As JBJS media offerings continue to grow, Your Case Is On Hold is now the featured podcast for insights into each issue of JBJS. Co-hosted

This Resident Roundup post comes from Sean Pirkle, MD. He offers his candid perspective on a question that other residents may also find themselves pondering.
JBJS is pleased to announce the publication of the JBJS Supplement on Large Database and Registry Research in Joint Arthroplasty and Orthopaedics. The supplement was
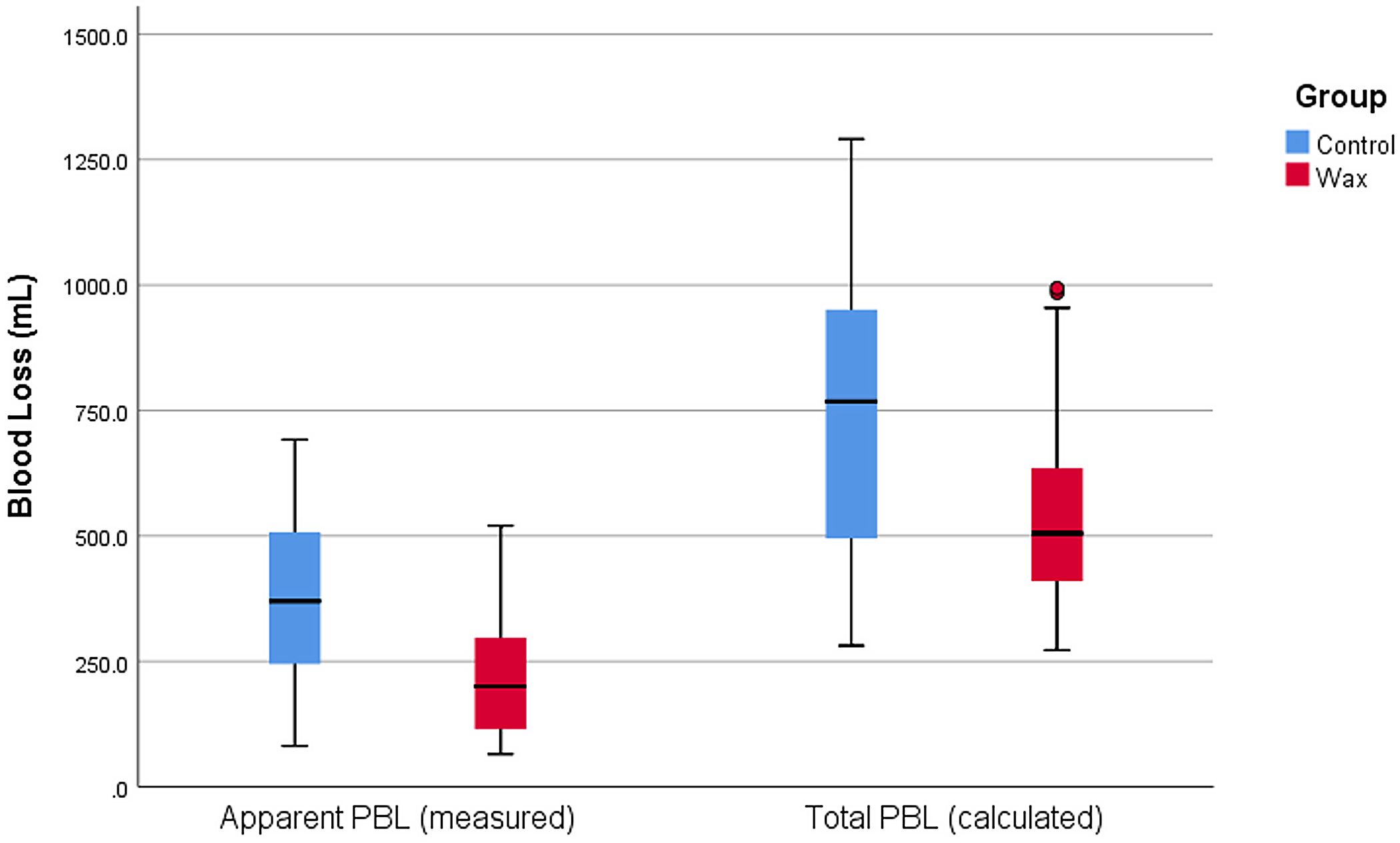
A number of measures have been suggested for reducing perioperative blood loss (PBL) in total hip arthroplasty (THA). A new randomized clinical trial in JBJS