Hip dysplasia is known to cause early joint deterioration, instability, and pain. It can be corrected with the Bernese periacetabular osteotomy (PAO). However, stability of
Tag: periacetabular osteotomy
Hip preservation continues to be a “hot topic.” Many deformities can be addressed surgically by normalizing hip biomechanics and preventing further degeneration. Legg-Calvé-Perthes (LCP) disease
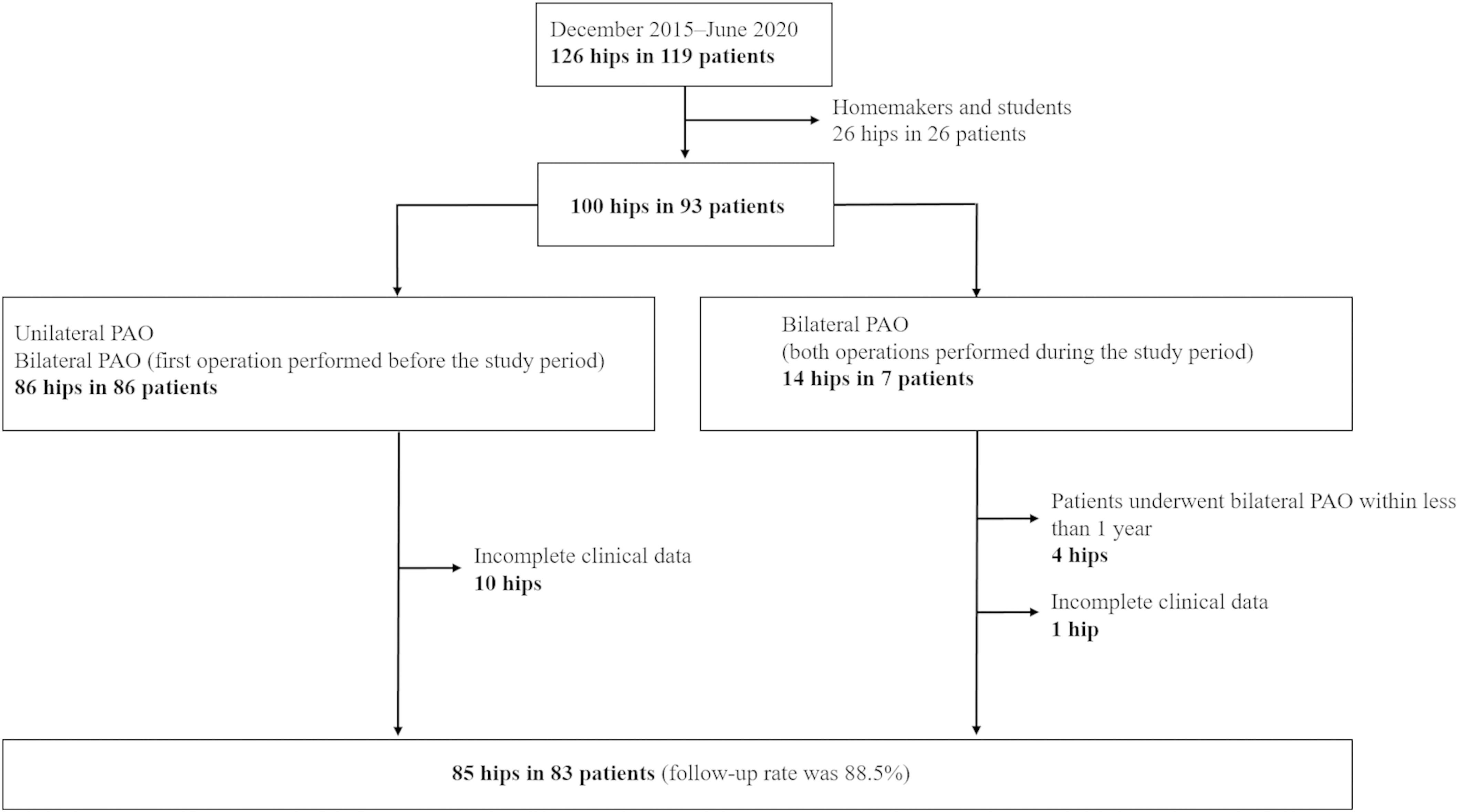
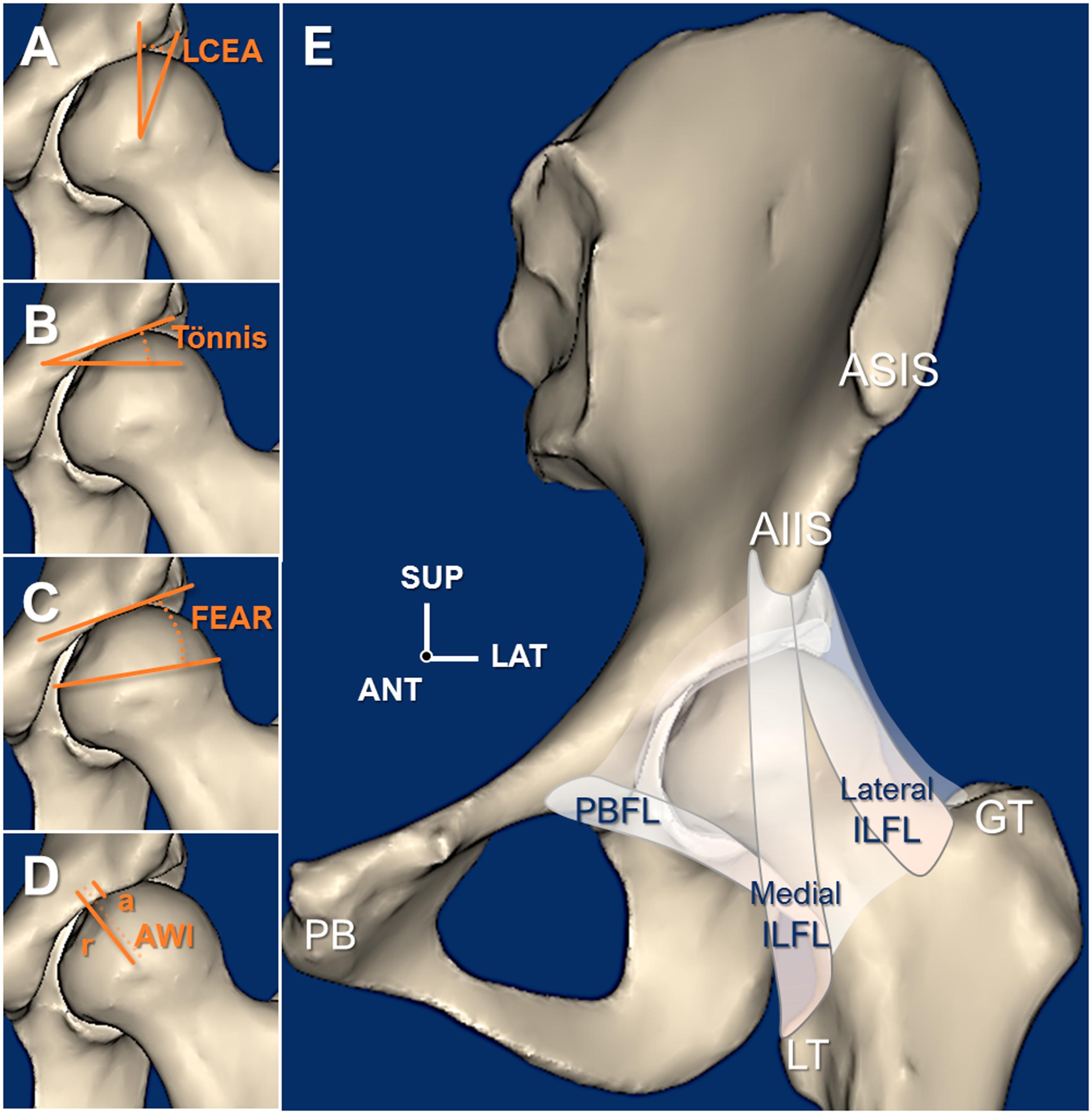
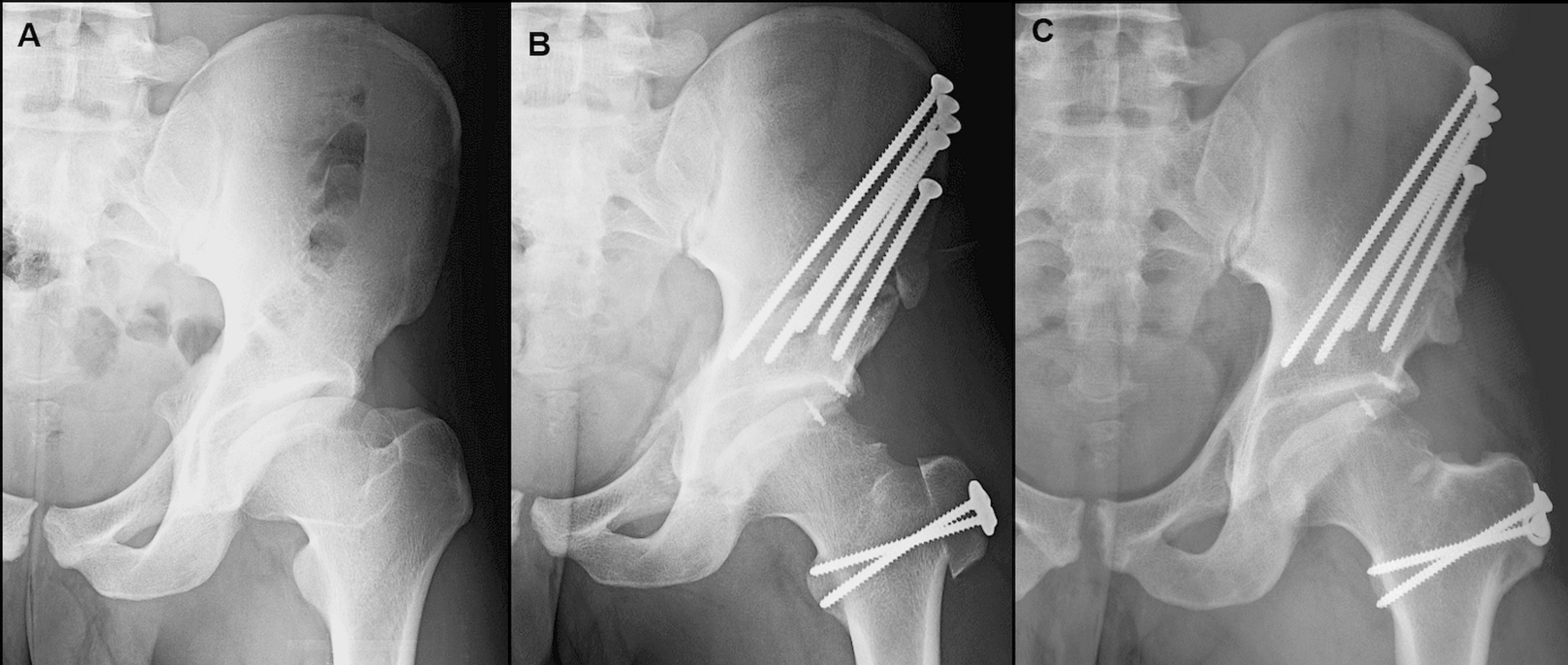
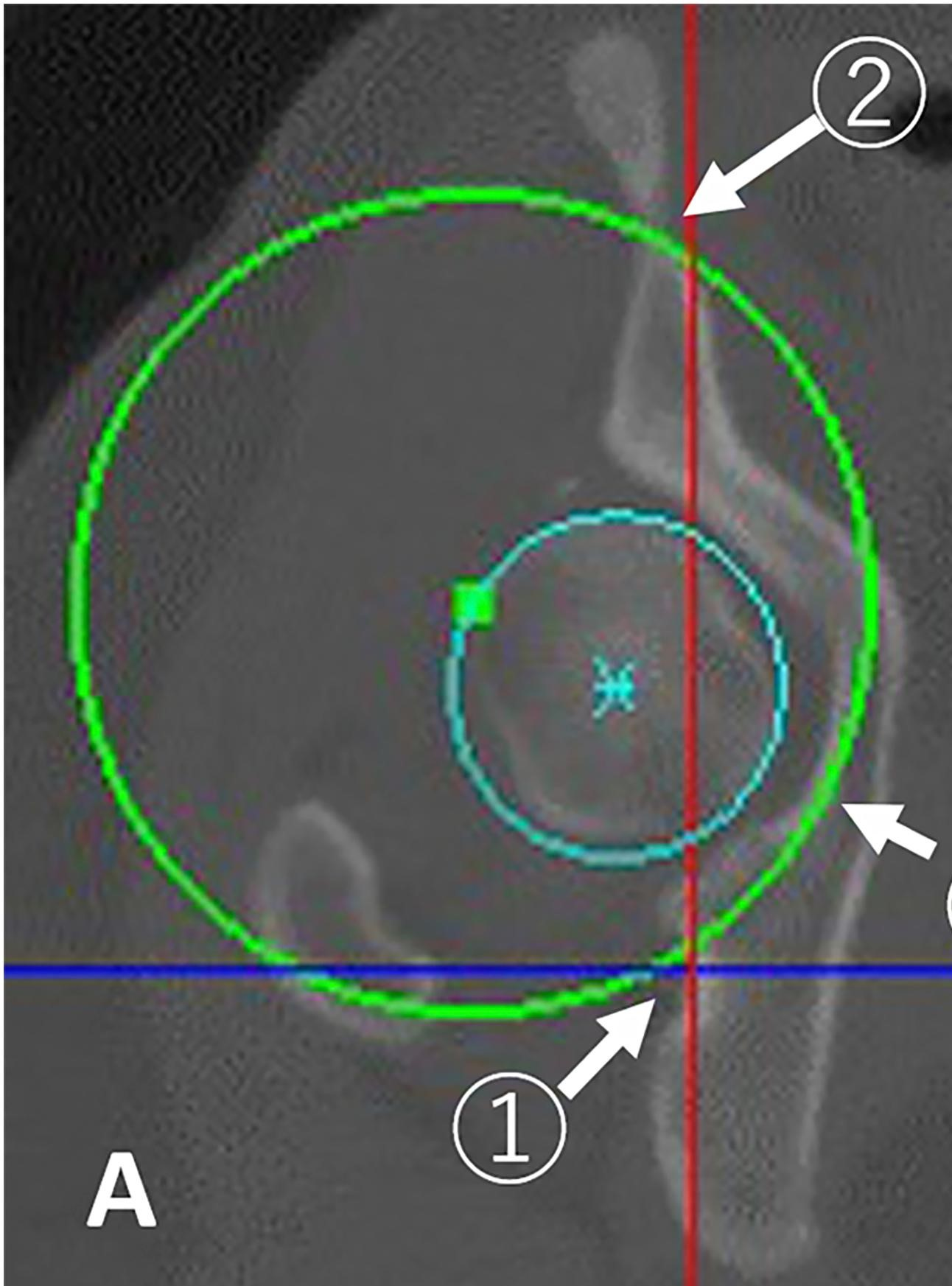
A periacetabular osteotomy (PAO) is a surgical treatment for hip dysplasia that has been shown in adult patients to delay the onset of hip arthritis
As surgeons, we are always looking to improve, or at least we should be. How can we obtain better outcomes? How can procedures be more time efficient? Can
JBJS Essential Surgical Techniques (EST) is pleased to congratulate the winners of its two Editor’s Choice Awards for 2017: The award for best surgical-technique article went
The treatment of hip dysplasia in patients with Down syndrome is challenging. Until the March 7, 2018 issue of JBJS, only short-term results from periacetabular
The Bernese periacetabular osteotomy (PAO) has become the procedure of choice for treating symptomatic acetabular dysplasia. But how long-lasting are its benefits? Quite, according to
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties.