Recent studies on periprosthetic joint infection (PJI) and other topics are presented in the JBJS Guest Editorial “What’s New in Musculoskeletal Infection.” Here, we spotlight
Tag: periprosthetic joint infection

Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. This month, co-author
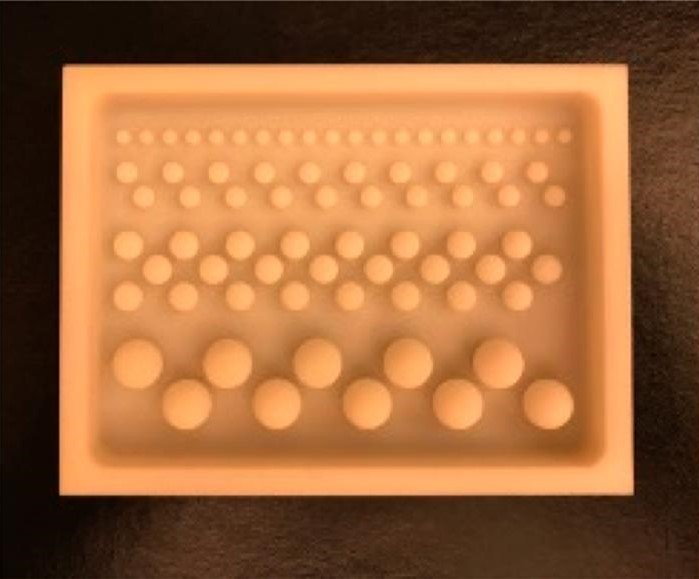
The incorporation of antibiotics within polymethylmethacrylate (PMMA) has been widely used over recent decades for managing infection following skeletal trauma. Early research helped to

Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 14 subspecialties. Click
I was once told that if you don’t have any cases with complications, you either aren’t operating enough or aren’t following your patients. Although we
In June 2019, OrthoBuzz reported on the FDA approval of a rapid, lateral-flow alpha defensin test that helps detect periprosthetic joint infections (PJIs) from synovial
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a
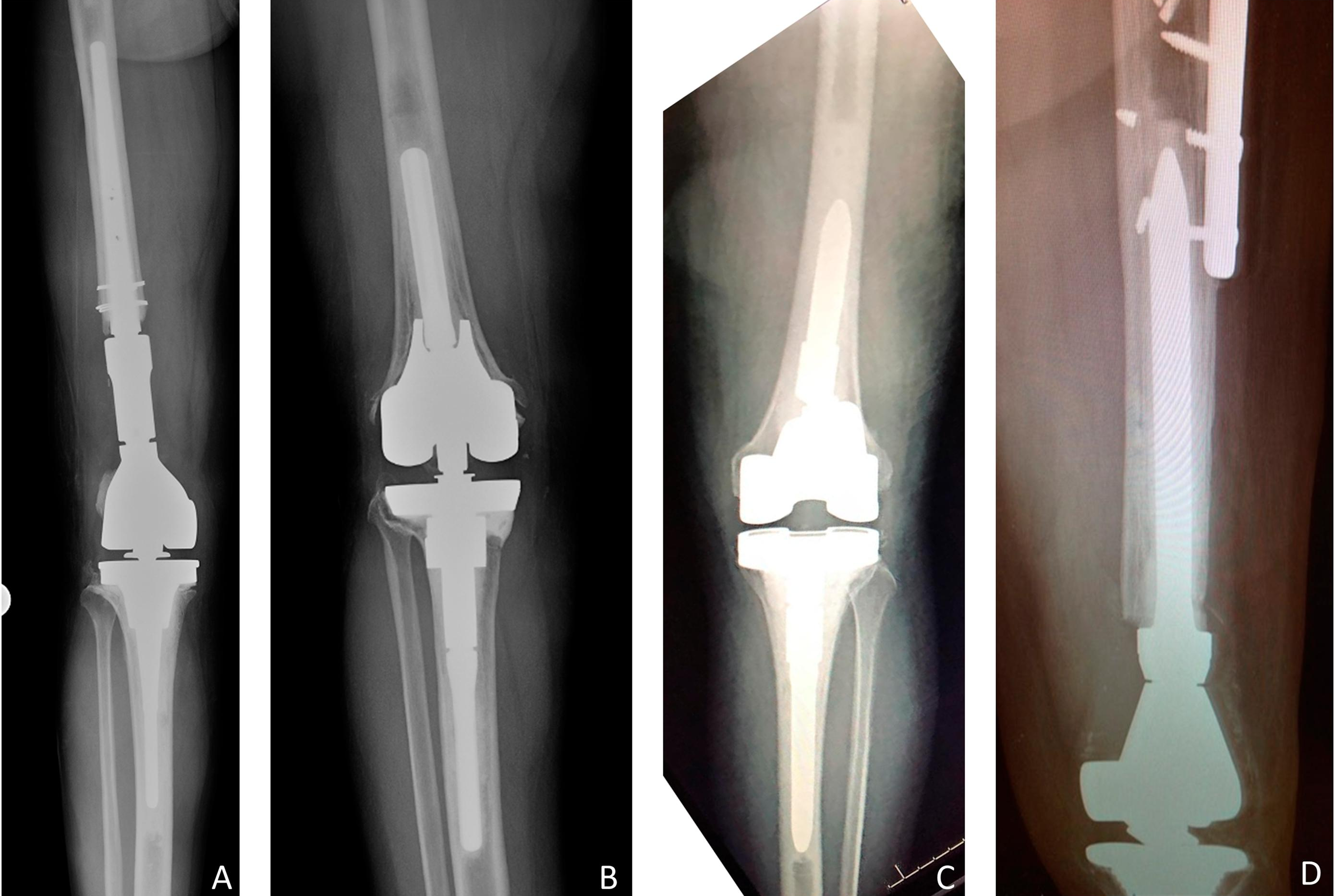
It’s hard to contemplate “conservative treatment” in the case of a revised total knee arthroplasty (rTKA) with extensive instrumentation that needs a reoperation due to
We recently celebrated Veteran’s Day with the annual tradition of rightfully honoring the men and women who have served in the Armed Forces. After their
Every month, JBJS reviews the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a collection