JBJS video summaries provide helpful synopses of key data from scientific studies. A video summary is now available with the new JBJS study by Sinclair
Tag: total knee arthroplasty
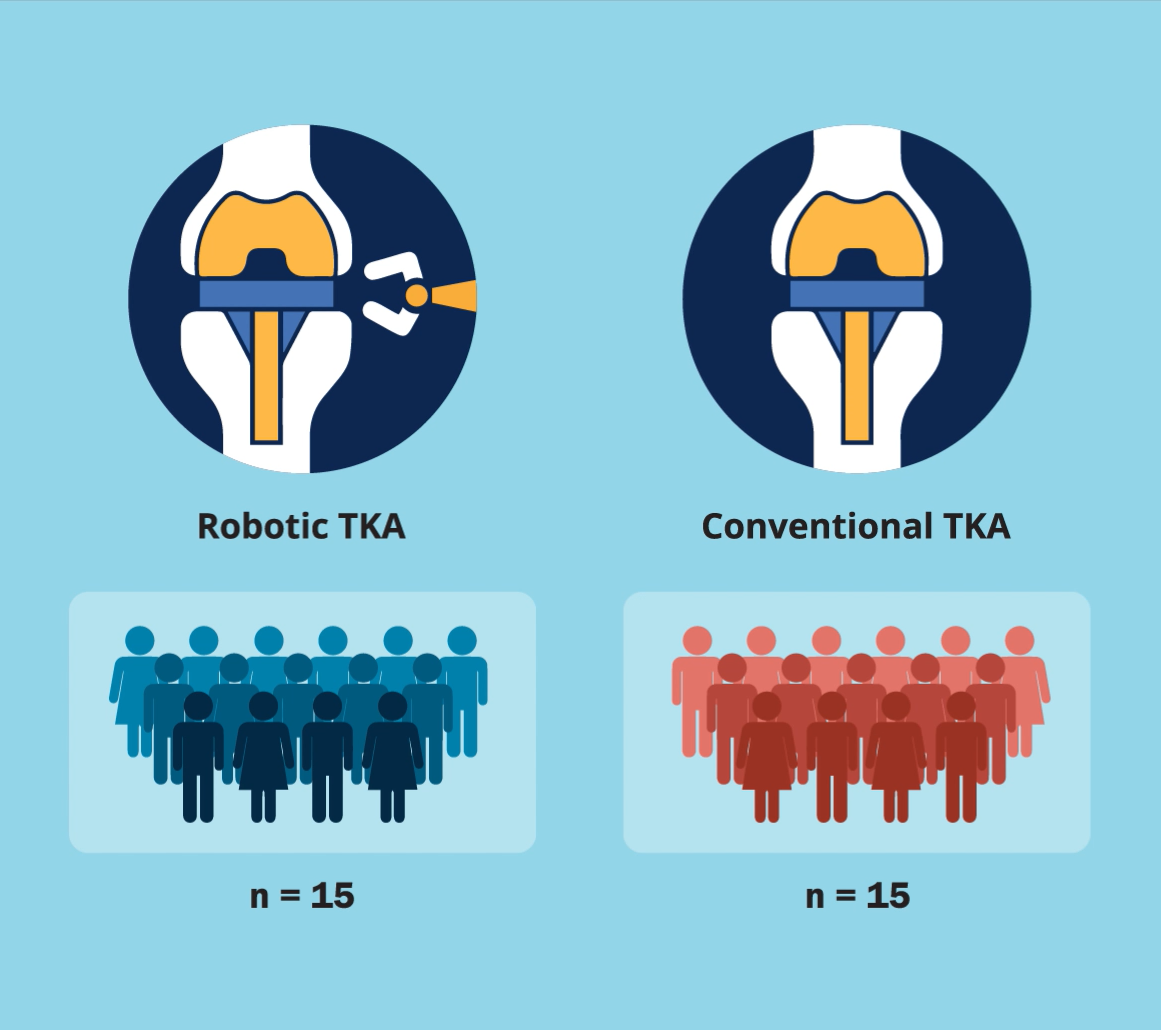
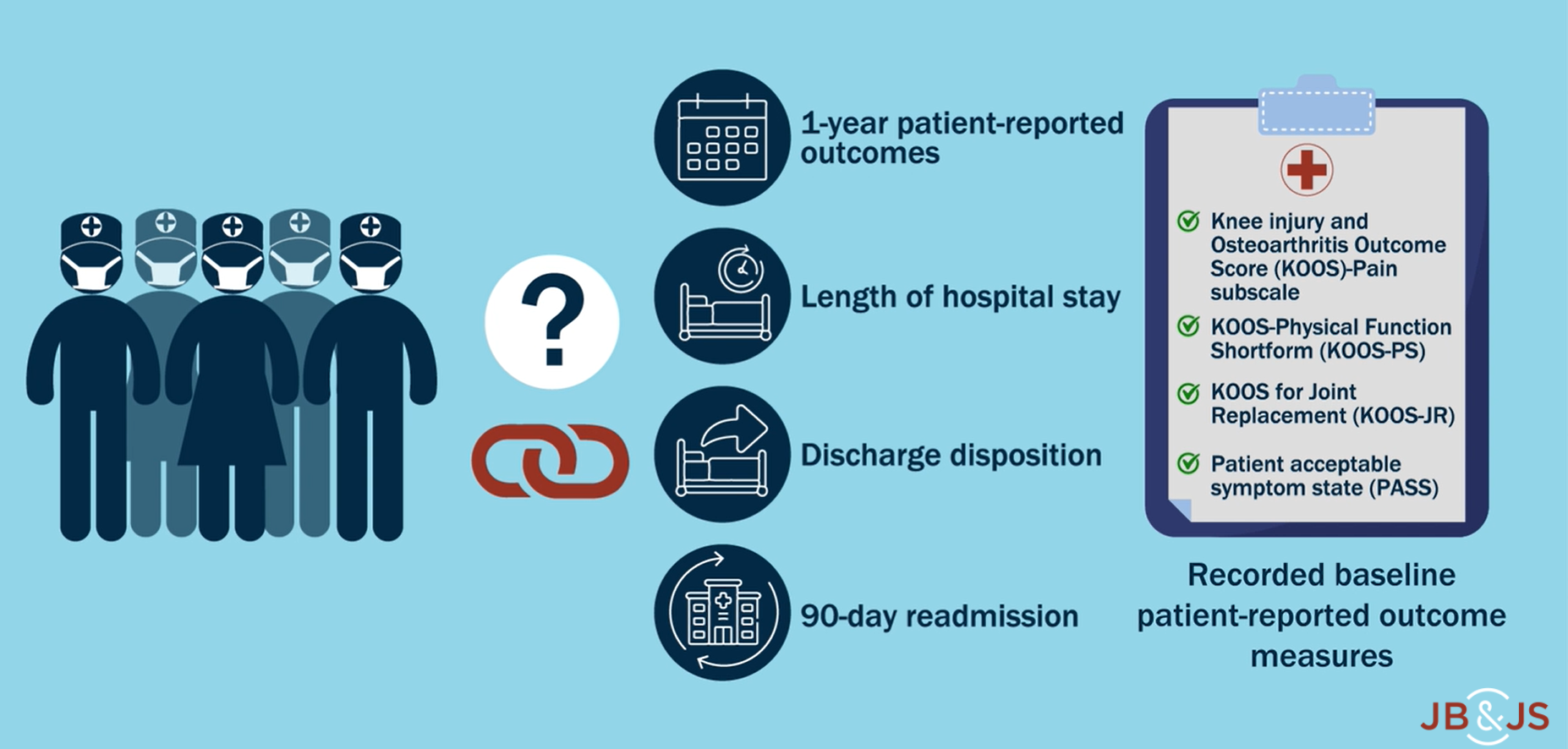
A new JBJS study by Fontalis et al. compares the inflammatory response in robotic-arm-assisted total knee arthroplasty (TKA) vs. conventional jig-based TKA. The investigators also
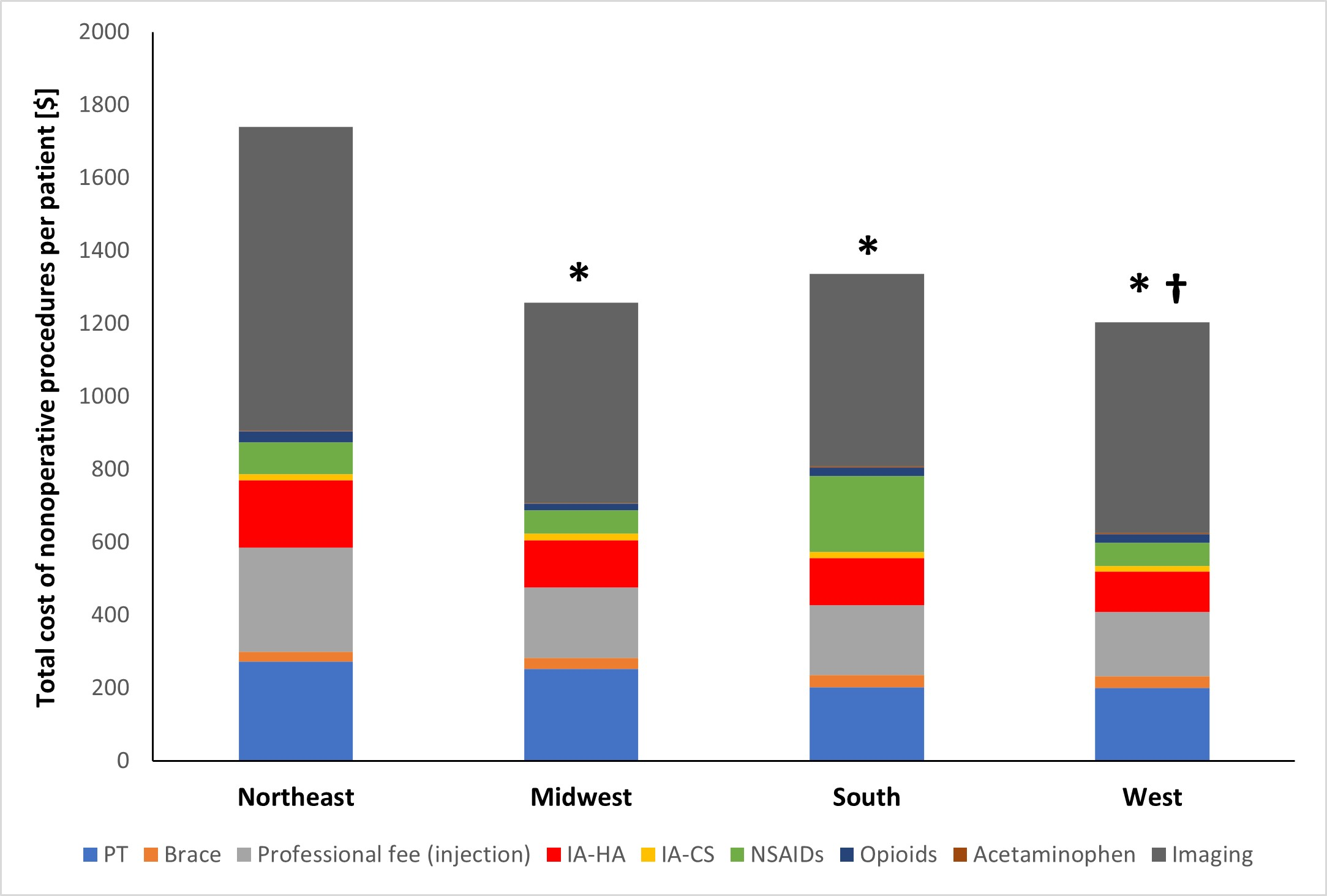
A new JBJS study reviews costs associated with nonoperative management of osteoarthritis in the 1-year period leading up to total knee arthroplasty (TKA). JBJS Deputy

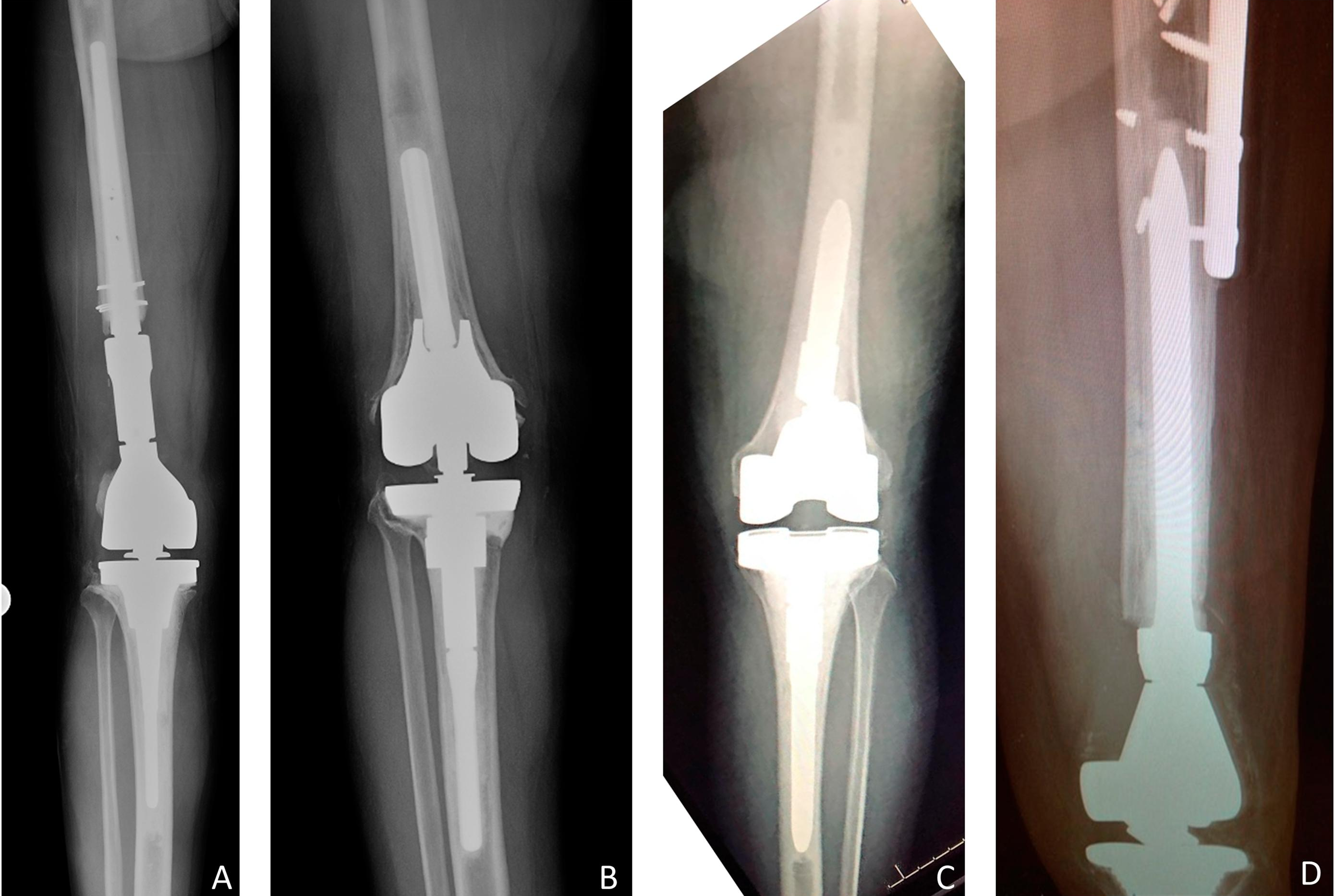
In the current issue of JBJS, Goh et al. report on the association between glucose variability and postoperative complications following aseptic revision total joint arthroplasty
Recent studies on periprosthetic joint infection (PJI) and other topics are presented in the JBJS Guest Editorial “What’s New in Musculoskeletal Infection.” Here, we spotlight

Intra-articular hyaluronic acid injections, also known as viscosupplementation, are a common treatment option for many patients with end-stage osteoarthritis of the knee. However, the effectiveness

OrthoBuzz is pleased to announce the winners of the JBJS Essential Surgical Techniques (EST) Editor’s Choice Awards. Two EST awards are given: for the best
This guest post comes from Jaime Bellamy, DO in response to a recent randomized clinical trial reported in JAMA Network Open and featured in MedPage

Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. This month, co-author
Genetic susceptibility to orthopaedic conditions is of interest to clinicians and patients alike. While the link between genetics and certain pediatric conditions is known, studies