The importance of LGBTQ+ representation in orthopaedic surgery and the formation of Pride Ortho are the focus of a current JBJS Orthopaedic Forum article. “New
Tag: diversity

A recent JBJS report by Stein et al. calls attention to the important topic of physician mental health. In particular, the authors sought to determine
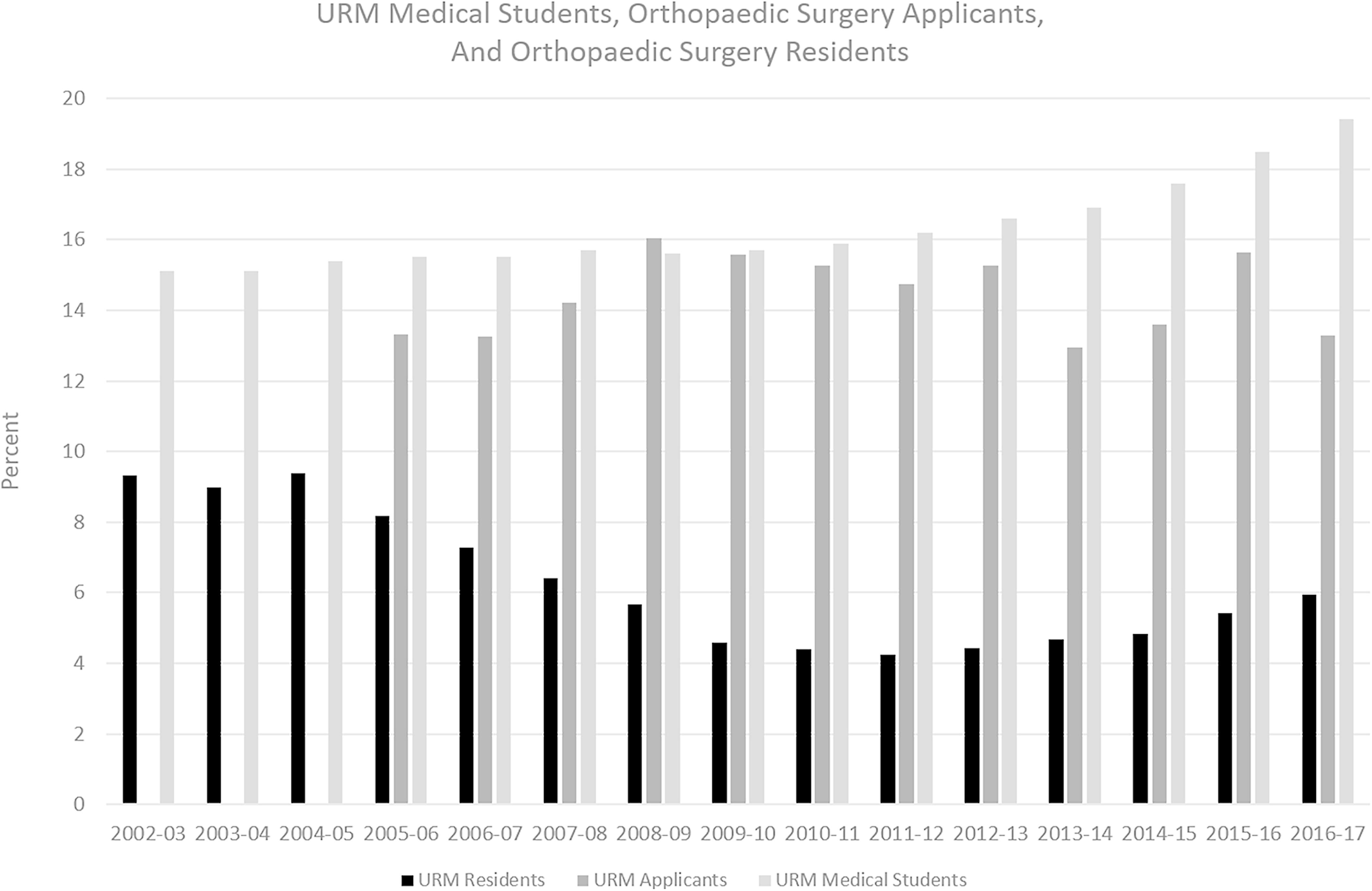
There is a long-standing crisis in the field of orthopaedics with respect to diversity, equality, and inclusion. It rightly has garnered press, including research articles

The American Orthopaedic Association (AOA) and its Council of Orthopaedic Residency Directors (CORD) recently issued a Statement of Support for Inclusivity in response to highly alarming comments in a crowd-sourced file circulated among medical

This guest post comes from Jennifer Beck, MD. As a female, mid-career orthopaedic surgeon, I believe I bring a unique perspective to reporting on the changes that I have witnessed over the past 15
Residency training is an essential pipeline to keeping the field of orthopaedics strong. As I tell the surgeons in my department, we should always be
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes Christopher Dy, MD, MPH in response to 2 recent studies in JBJS Open Access. It’s that
In 2016, only 6.5% of practicing orthopaedic surgeons in the US were women. By contrast, 49% of all medical students in the US are women.
On Wednesday, November 14, 2018 at 8:00 PM EST, the American Orthopaedic Association (AOA) and The Journal of Bone & Joint Surgery (JBJS) will co-host a one-hour complimentary
On Wednesday, November 14, 2018 at 8:00 PM EST, the American Orthopaedic Association (AOA) and The Journal of Bone & Joint Surgery (JBJS) will co-host a one-hour complimentary

