In a new study in JBJS, Anderson et al. provide enlightening data on total joint arthroplasty (TJA) utilization in the setting of Medicare Advantage (MA) compared with traditional Medicare. A related editorial by Jeffrey N. Katz, MD, MSc, and Daniel Betensky, AB, offers further reflections on the investigation. The study and editorial are available at JBJS.org:
Medicare Advantage Is Associated with Lower Utilization of Total Joint Arthroplasty
Editorial: Total Joint Arthroplasty Utilization in Persons Over 65 Years of Age. Advantage Medicare?
The researchers note that approximately one-half of Medicare beneficiaries receive their coverage through MA plans. These plans use managed care techniques to control costs, with health maintenance organizations (HMOs) and preferred provider organizations (PPOs) commonly serving as structures for implementing the cost-containment strategies1,2.
It is not clear, say the researchers, whether MA insurers limit utilization of high-value surgical procedures such as TJA. They sought to explore the question of utilization in a cross-sectional study that used a 20% sample of 2018 traditional Medicare claims and MA encounter records for enrollees 65 to 85 years of age.
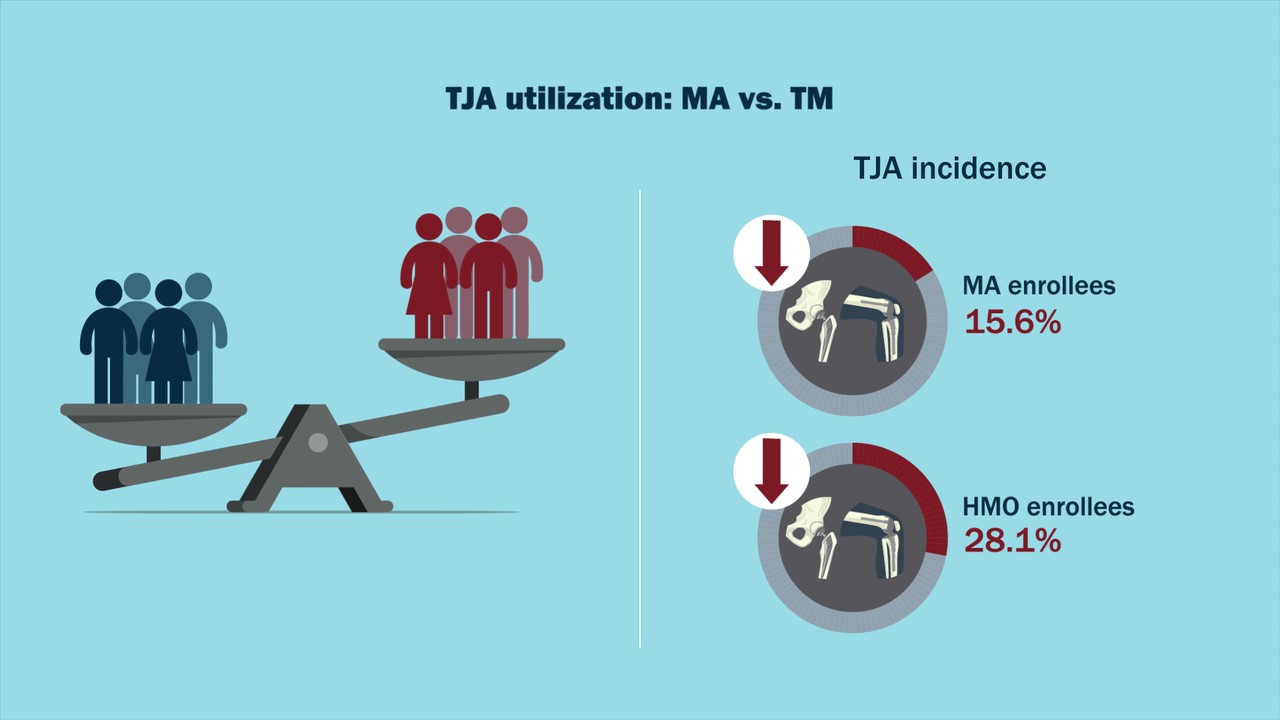
Briefly, they found a 15.6% lower incidence of TJA for MA vs. traditional Medicare enrollees. Furthermore, HMO enrollees were 28.1% less likely to undergo TJA than those covered by traditional Medicare. MA was also associated with a longer time to both orthopaedic surgeon evaluation and surgery. Two years following a diagnosis of osteoarthritis, 10.4% of enrollees in traditional Medicare had undergone inpatient TJA compared with 7.9% of PPO and 5.7% of HMO enrollees. Watch the related video abstract of this study.
In their editorial, Katz and Betensky probe several noteworthy questions raised by the study findings. “These lingering questions notwithstanding,” they write, “the important message of this study is that TJA, a highly efficacious and cost-effective, although costly, procedure, is used 28% less frequently among MA HMO enrollees than among TM [traditional Medicare] enrollees. As noted in Table I in the article by Anderson et al., the persons affected by this disparity in utilization are most likely to be Black, Hispanic, poor, and beset with chronic comorbid conditions. Thus, these data suggest a potential mechanism for health-care utilization disparities in the Medicare population: low premium costs attract vulnerable populations to MA HMOs, which, in turn, restrict the use of costly (although high-value) procedures, such as TJA. Claims data do not permit us to determine if this difference in utilization translated to lower quality of life among those who did not undergo TJA, although it is widely recognized that TJA typically improves quality of life dramatically. Future studies should seek to investigate the presence of disparities in health outcomes between TM and MA (HMO and PPO) enrollees ….” Read the full editorial here.
For more insights on this study and others, check out Your Case Is On Hold, a JBJS podcast with Drs. Antonia Chen and Andrew Schoenfeld, who discuss articles in the current issue of JBJS.
References
- Anderson KE, Wu RJ, Darden M, Jain A. Medicare Advantage Is Associated with Lower Utilization of Total Joint Arthroplasty. J Bone Joint Surg Am. 2024 Feb 7;106(3):198-205. Epub 2023 Nov 16.
- Katz JN, Betensky D. Total Joint Arthroplasty Utilization in Persons Over 65 Years of Age: Advantage Medicare? J Bone Joint Surg Am. 2024 Feb 7;106(3):177-79.



Great summary of an important study.