The recent JBJS Guest Editorial “What’s New in Osteoporosis and Fragility Fractures” provides an update on this important area of orthopaedic research. The authors review
Tag: JBJS

…to apply for the JBJS Robert Bucholz Journal Club Support Program for the 2022-23 academic year. Applications are due by September 30, 2022. Journal Club
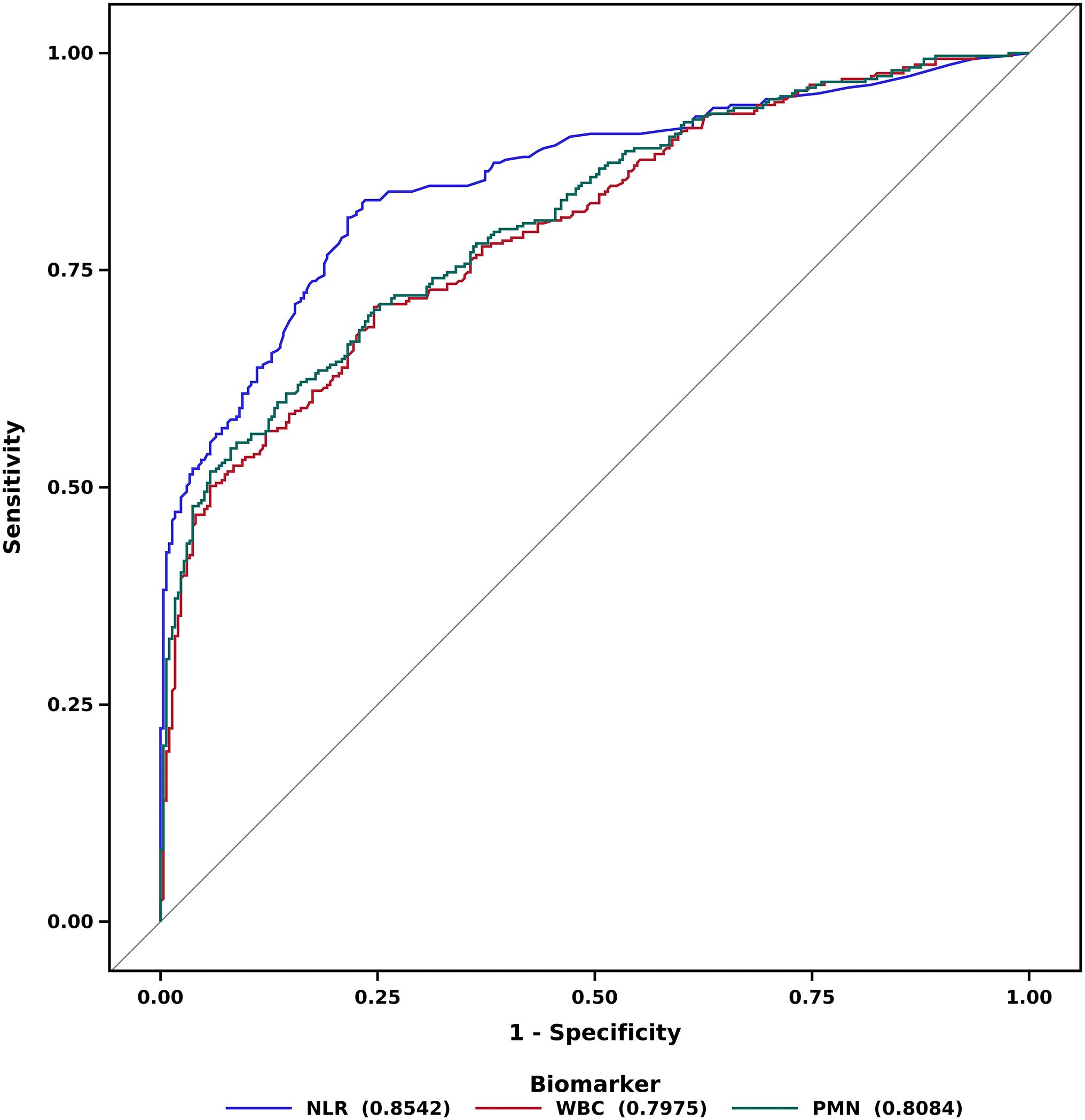
There are some orthopaedic conditions for which a delay in treatment of even a few hours can lead to poor outcomes. Septic arthritis (SA) is
JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers
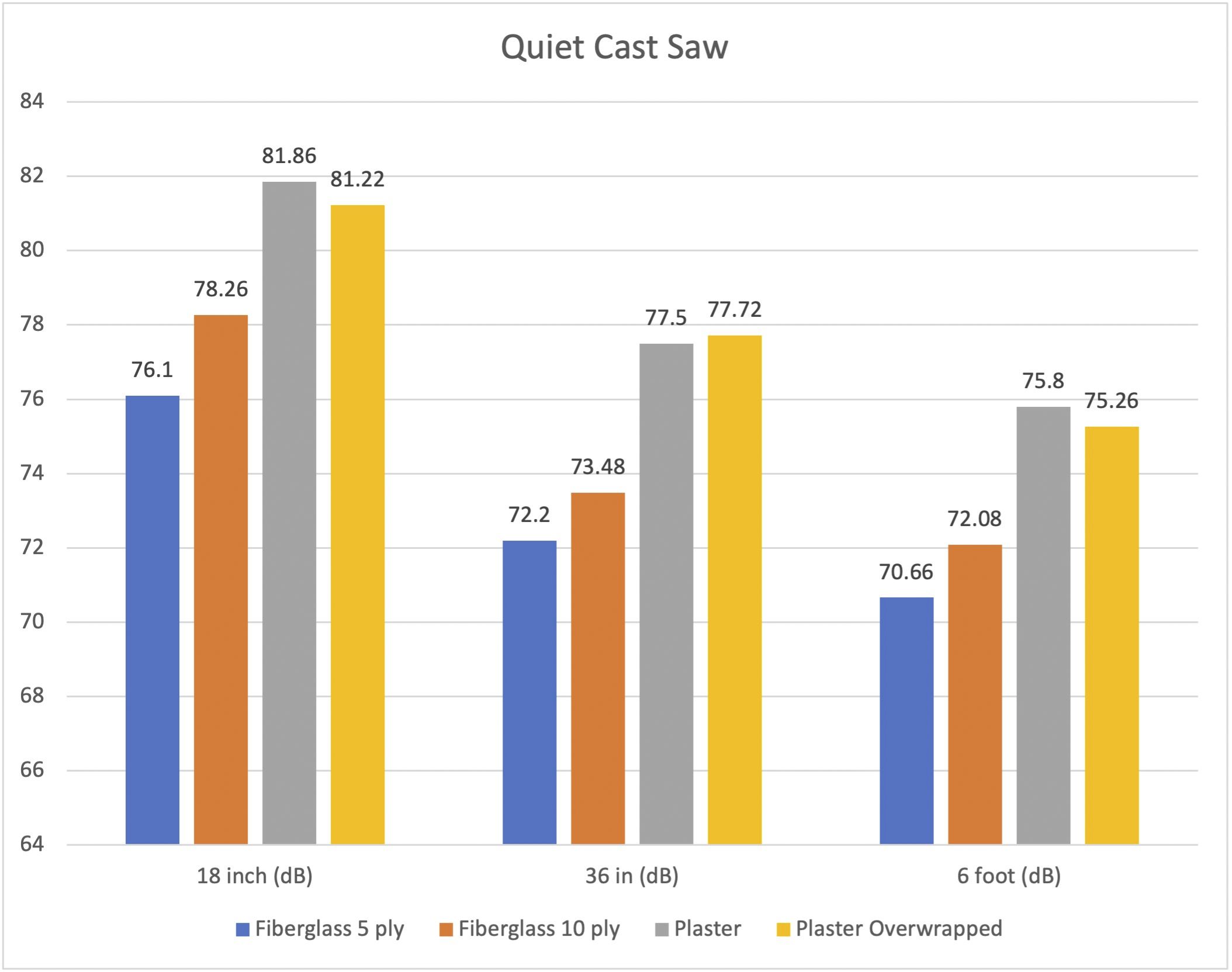
A new study in JBJS examines noise levels during cast removal. In this post, JBJS Editor-in-Chief Dr. Marc Swiontkowski reflects on the importance of research

JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers

The rise in health-care costs has contributed to the push for value-based health-care (VBHC) reform. A recent JBJS-AOA Critical Issues article by Lin et al.
JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers

Each month, JBJS publishes a review of the most pertinent studies from the orthopaedic literature in a select subspecialty. Here, we spotlight 5 of the 75 papers featured

JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers

