Rotator cuff repair, shoulder arthroplasty, shoulder instability, and the treatment of elbow injuries are among the topics of recent studies reviewed in the new JBJS
Tag: total shoulder arthroplasty
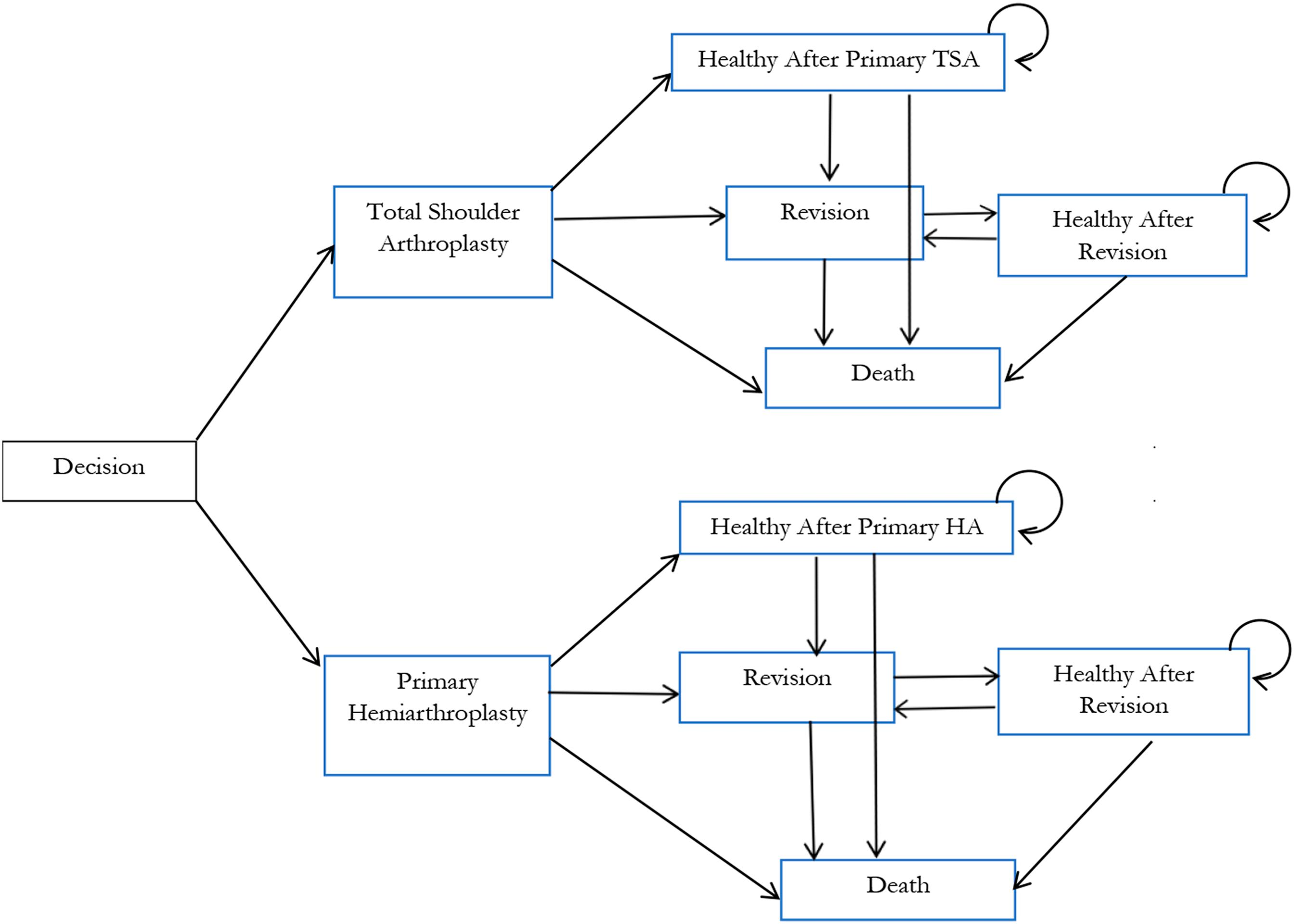
In a new study reported in JBJS, Lapner et al. conducted a cost-utility analysis of total shoulder arthroplasty (TSA) versus hemiarthroplasty from the perspective of Canada’s publicly funded health-care system. They used
The analysis did not identify evidence that the results of TSA were statistically or clinically improved over the 2 decades of study or that any
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Andrew D. Duckworth, MSc, FRCSEd(Tr&Orth), PhD, in response to a recent study in JBJS. Propionibacterium acnes
The relative roles of bones and muscles in joint pathologies are often difficult to tease apart. In the March 7, 2018 issue of The Journal,
Under one name or another, The Journal of Bone & Joint Surgery has published quality orthopaedic content spanning three centuries. In 1919, our publication was
Although the indications for anatomic and reverse total shoulder arthroplasty (TSA) are different, better understanding of the rate of improvement with each type of surgery
Shoulder surgery for complex conditions such as irreparably large rotator cuff tears has been revolutionized by the concept of reverse total shoulder arthroplasty (rTSA). Improved
In the April 19, 2017 issue of The Journal, Cancienne et al. compare complication and readmission rates for patients undergoing ambulatory shoulder arthroplasty with those
Anecdotally, many patients experience extreme discomfort after shoulder surgery. The April 5, 2017 issue of JBJS features results from a randomized controlled trial comparing morphine