This commentary comes from guest contributor Matthew Deren, MD, in response to a recent study in The New England Journal of Medicine. To cement or
Tag: hip fracture

When discussing patient outcomes of hip fractures, we often are speaking of fractures of the proximal part of the femur. But what about the other side of the hip joint, the acetabulum? Among fragility-related injuries, we’re seeing a rise in the incidence of acetabular fractures. And
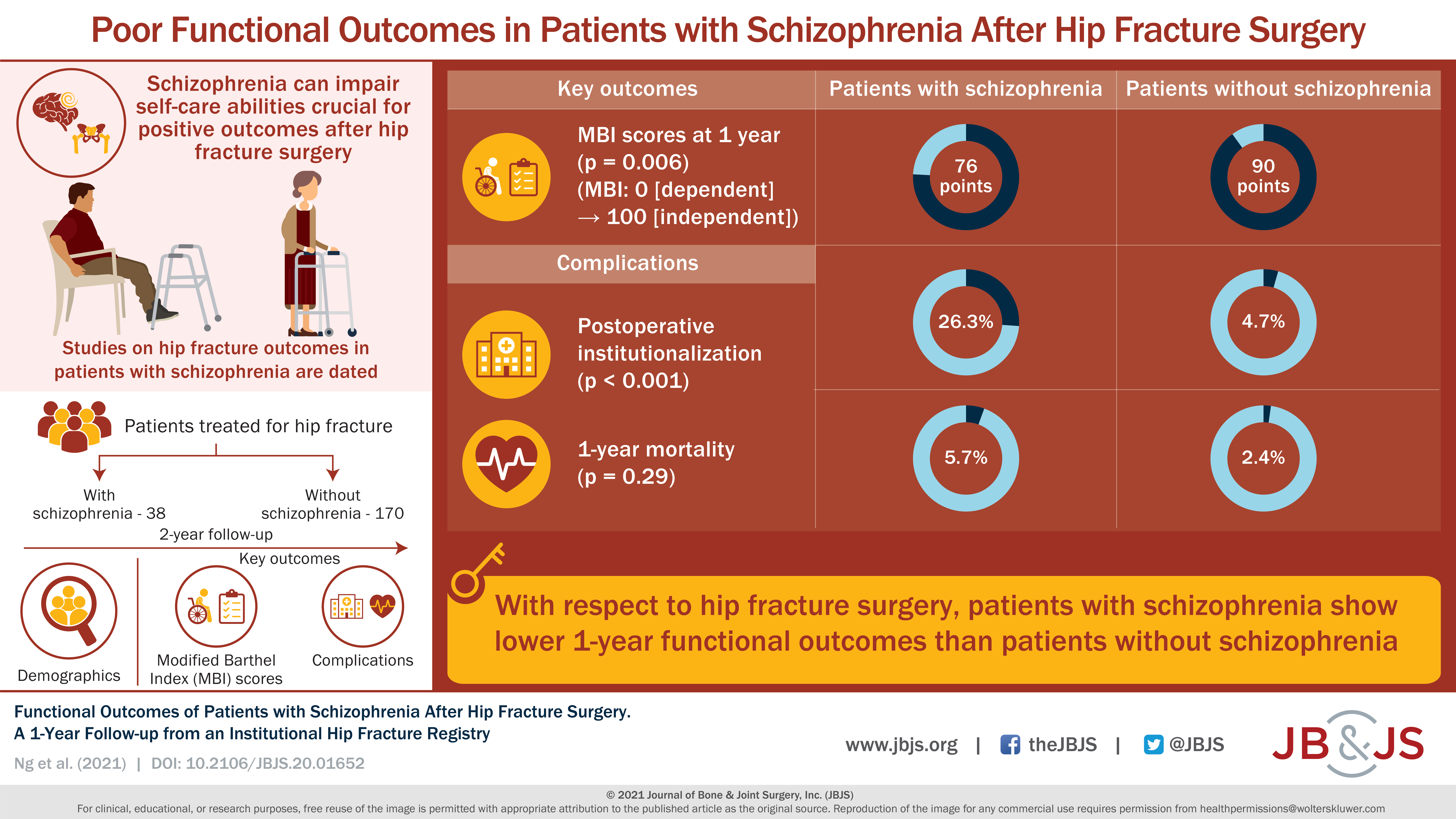
Thirty-eight patients with schizophrenia were compared with 170 geriatric patients without schizophrenia who underwent a surgical procedure for a hip fracture. Read the full article
The worldwide incidence of mental illness seems to be on the rise—and along with it a widespread recognition that this “epidemic” should receive at least
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from James Blair, MD, in response to a recent edition of the OrthoJOE podcast. Geriatric
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a
OrthoBuzz occasionally receives posts from guest bloggers. This guest post comes from Shahriar Rahman, MS in response to a recent study in JAMA Internal Medicine. Hip
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for
The benefits of peripheral nerve blocks for pain control and decreased use of opioids has been well-established for several orthopaedic procedures. In the May 20,
We have all come to realize that promising results from lab studies or preclinical trials in animal models do not always translate into meaningful clinical

