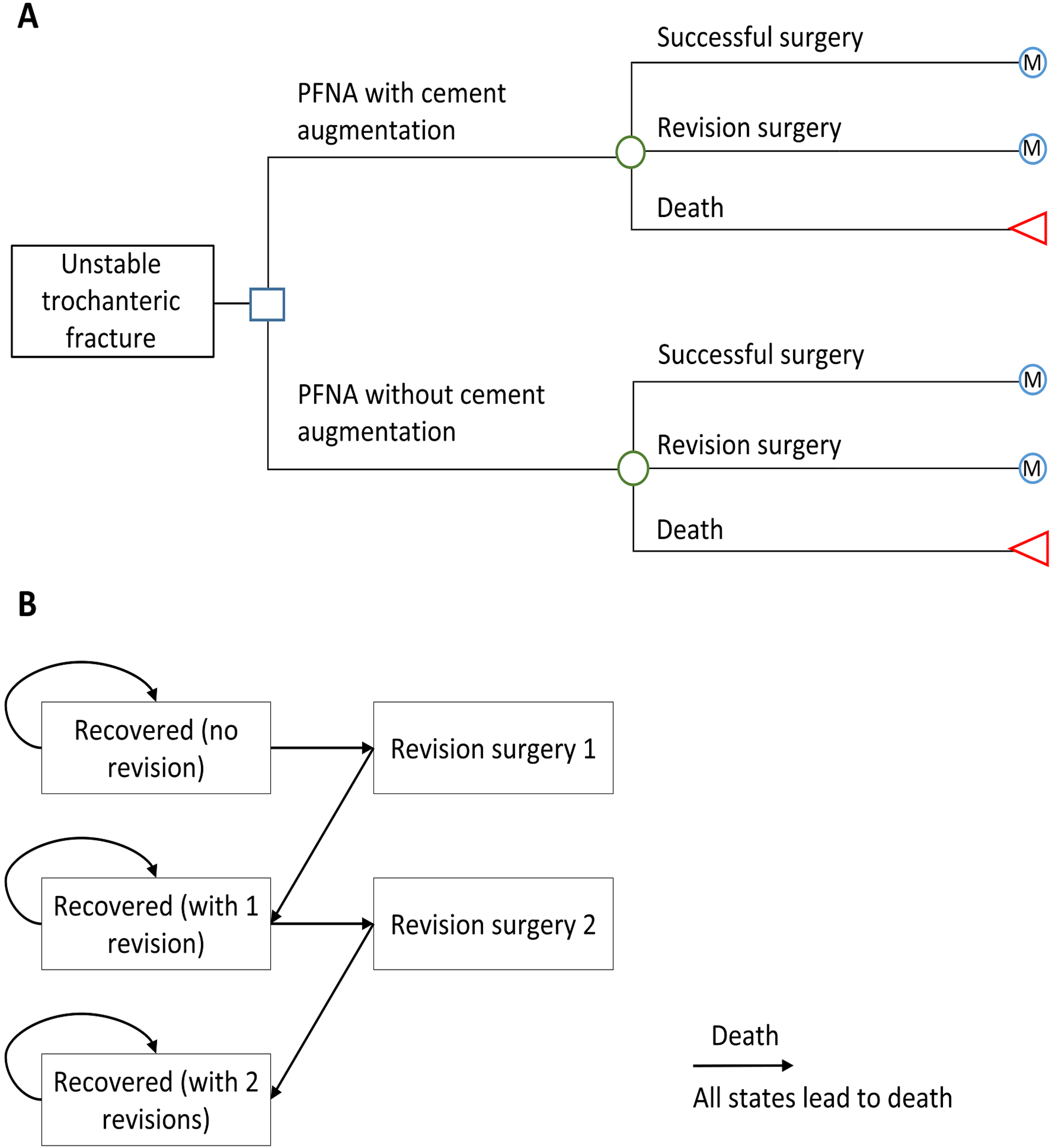
Trochanteric fractures often occur in older patients, including those with osteoporosis, and are associated with high rates of mortality and morbidity. Investigators previously conducted a
Tag: intramedullary nail
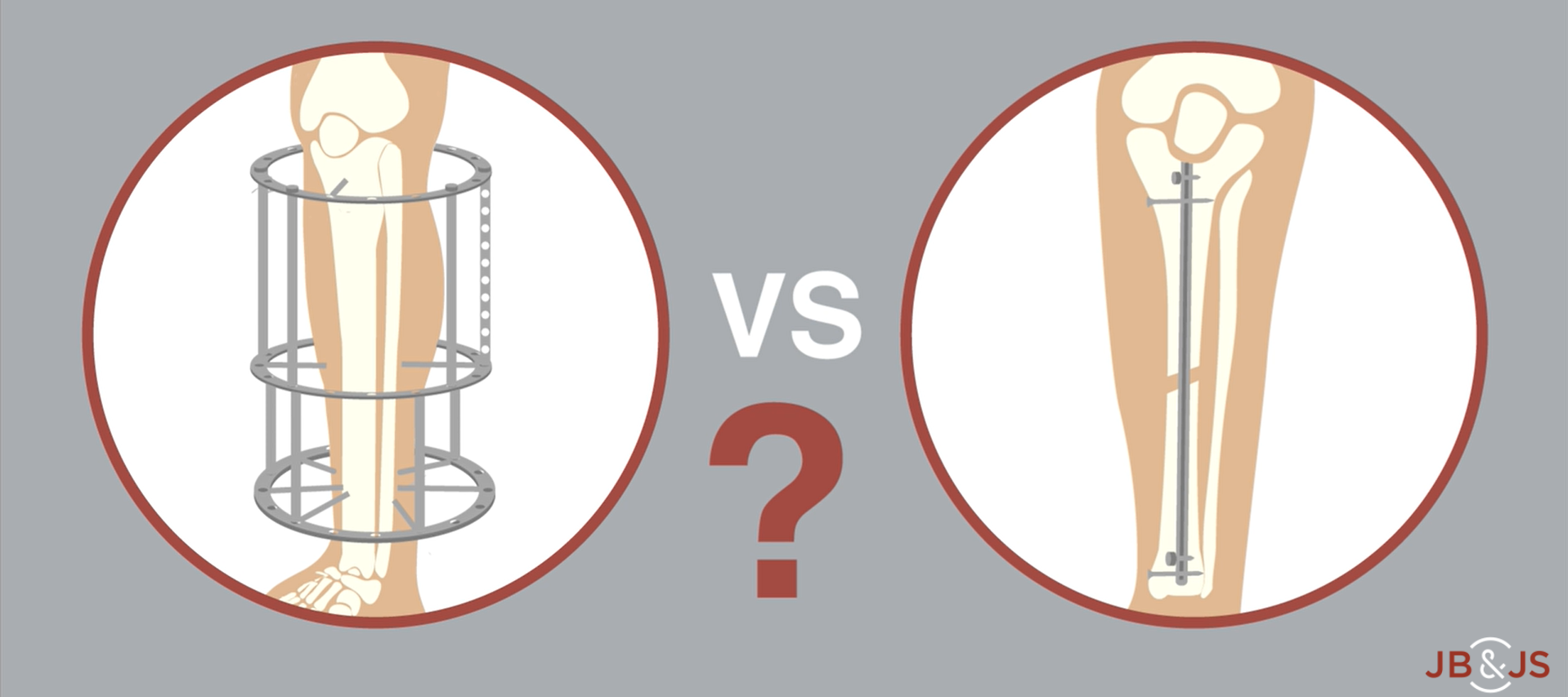
A new RCT provides Level I evidence for internal vs. external fixation of severe open tibial fractures. High-level data have been lacking until now. In
In our ongoing attempt to identify pharmacologic interventions that improve fracture healing, the sclerostin inhibitor romosozumab is a logical candidate, as it has been shown
Generally speaking, orthopaedic surgeons in low-resourced environments deliver the best care for their patients with skill, creativity, and passion. These surgeons are accustomed to scrambling
I’ll be honest: I have never worried much about breakage of the cephalomedullary nails I implant for proximal femur fractures. Instead, I’m focused on the
Orthopaedic surgeons and their staffs are aware of the paradigm shift that has taken place in the last 10 to 15 years regarding the treatment
Under one name or another, The Journal of Bone & Joint Surgery has published quality orthopaedic content spanning three centuries. In 1919, our publication was
In the March 1, 2017 edition of The Journal, Eliezer et al. report on their experience managing femoral fractures in a major treatment center in
We posted our first “Case Connections” article about bisphosphonate-related atypical femoral fractures (AFFs) one year ago. Since then, JBJS Case Connector has published three additional case reports on
In the December 2, 2015 issue of The Journal, Reindl et al. report on the results of a multicenter randomized trial comparing intramedullary (IM) fixation